tl;dr: In many organizations, “accountability” is code for blame and punishment. Lean leadership redefines accountability as improving systems, clarifying expectations, and helping people succeed rather than singling them out for failure.
“Accountability” is a word that's easy to throw around in an organization. It's often pretty meaningless (or not well understood). What does it really mean?
People say things like:
“We need a culture of accountability.”
“We need to hold people accountable.”
What Leaders Usually Mean When They Say “Accountability”
When I hear that phrase, I like to call time out and ask, “What do you mean exactly? Give me an example of what you mean.”
People often don't know. They just throw around that phrase.
Talking about accountability sounds nice. Leaders love talking about holding others accountable, even if they're not personally being accountable for much of anything.
When Accountability Becomes Blame
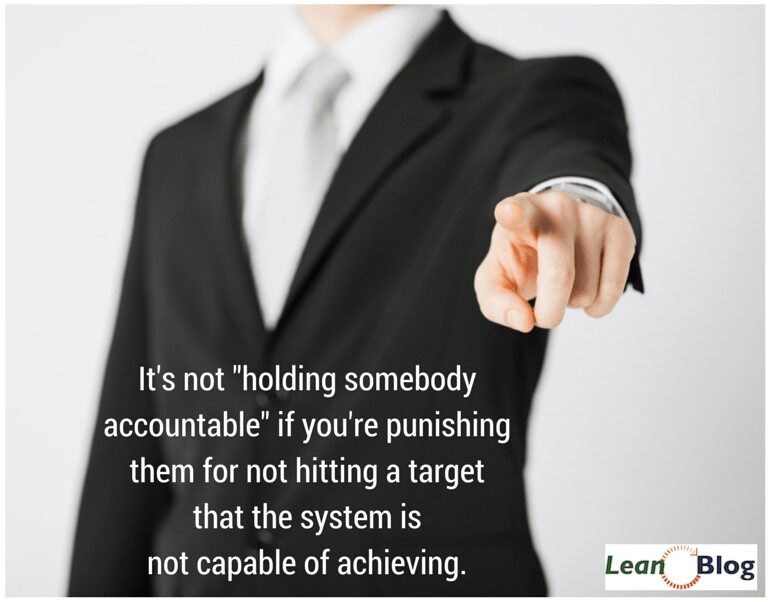
Unfortunately, in practice, the word “accountability” is often corporate speak for “let's blame and punish people.”
Nobody intentionally says things like:
“We need a culture of blaming and punishing people for systemic problems.”
or
“We need to blame and punish people.”
But that's often what's being done under the guise of “accountability.” It's a code word, a way of saying the things that aren't supposed to be said.
What does the word accountability even mean?
A dictionary definition says “accountable” means:
: required to explain actions or decisions to someone
: required to be responsible for something
Why You Can't Hold People Accountable for System Problems
Accountable… to give an account… to explain actions or results. Can we really ask front-line staff to explain (or be responsible) for system problems like emergency department waiting times? Can we ask front-line managers to be accountable for systemic problems?
When leaders throw out a solution, such as “we need more accountability,” how do we know that “lack of accountability” is really a root cause of the problem at hand?
Saying “we need more accountability” is sort of a polite, coded way of saying “my people aren't trying hard enough” or “my employees don't care.” Those things are usually untrue, by the way. And these are awful things to say.
Instead of “more accountability,” we need to work together to improve the system that people are working in.
I think the list of things that people can “be held accountable for” is pretty limited. What are the things you really have control over? Maybe you can hold somebody accountable for showing up to work on time more often than not (although an unexpected system problem might occasionally interfere). If an employee is often five or ten minutes late to work because of traffic, they can be “held accountable” and take action to leave home earlier (even if that means arriving early some days).
Listen to Mark read this post (Learn more):
How Blame Distorts Metrics and Behavior
But in more complex situations, it's harder to simply hold people accountable. When we blame and punish people for not hitting targets, senior leaders might think they are “holding people accountable.” Look at situations like the 4-hour A&E waiting targets in the British NHS. People get blamed and punished, so they end up gaming the numbers and distorting the system (by holding patients just outside A&E to prevent the clock from starting or by admitting them after 3:55).
Senior leaders need to help people improve the system, not just hold them accountable.
Why are there long waiting times in A&E or the ED? It's often a systemic value-stream problem with root causes in outside agencies, such as long-term care or nursing homes, that lack capacity. This was a big problem when I worked with an Ontario hospital a few years back. The ED was all backed up. Why? Because they couldn't discharge enough inpatients. Why? Because there weren't enough long-term care beds in the community. Why? Because of government budget constraints.
No amount of “accountability” or blame for the ED or the hospital will fix that problem.
VA clinics were being held accountable for patient appointment waiting times, but the goal was deemed “unrealistic” by the federal government itself. It's unfair to hold people accountable for goals that are unattainable or beyond their control.
What Constructive Accountability Looks Like in Lean
Accountability isn't about blaming people for outcomes they don't control. It's about being clear on who owns which decisions, improving the systems that shape daily work, and responding to problems with learning instead of punishment. When leaders default to blame, people protect themselves, game the numbers, and hide problems. When leaders focus on systems, people speak up, experiment, and improve.
If an organization truly wants accountability, leaders must start by being accountable themselves–for the design of the system, the realism of the goals, and the behaviors they reward or punish. Lean doesn't eliminate accountability; it redefines it. Accountability in Lean means taking responsibility for making success possible, not for finding someone to fault when things go wrong.
That shift–from blame to constructive action–is where real improvement begins.
Also see this post from last year: Lean, Deming, and “Accountability.”
If you’re working to build a culture where people feel safe to speak up, solve problems, and improve every day, I’d be glad to help. Let’s talk about how to strengthen Psychological Safety and Continuous Improvement in your organization.








A funny “scapegoat” commercial
hat tip to Brian on Twitter
Often people are blamed with no consideration to the systemic problems.Is it not passing on the buck?
It is not fair.
Instead the leader must work together with the employee and solve the root cause of the problem.
This happens in a lean scenario under true ‘Lean Leadership’where the leader works with the employee and solves the root cause of the problem,inculcates a sense of ‘ownership’of the process with proper empowerment, rather than making him responsible for the process,no matter what process conditions are. And then the ‘Blame Culture’tends vanish…. !
Mark: really enjoy the audio versions of these blogs. This enables me to listen while commuting to work.
Years ago, I came across a few quotes that seem appropriate for your accountability blog:
“You can make excuses and you can make money – you can’t do both” (the late Richard Carlson, author of “Don’t Sweat the Small Stuff”.
“Fix the problem as opposing to affixing the blame”.
Lastly, the author Jim Collins wrote in “Good to Great” that great organizations conduct “autopsies without blame” to learn from mistakes and get better.
Ed – thanks for the comment and the quotes.
I’m glad you are enjoying the audio versions. It’s an experiment that I’ll likely continue because it doesn’t require much effort (I should already be proofreading my posts, anyway) and it might provide value to those with more listening time than reading time.
I’m curious – did you subscribe through iTunes or another method to get them automatically?
Mark
While it could be delivered as a cudgel. The accountability ladder is really a facile way of delegating, Offering to the people, all people that you are allowing them to make decisions. Delegating accountability will allow those willing to exercise leadership to act as drivers through those that are less likely to be willing to risk making mistakes.
That is a key in the accountability ladder, delivering the message in such away that each individual knows how much risk the company is willing to allow them, then the freedom for the people to make the best decision going forward. If they make a mistake, small coaching session to see that the message was delivered and the lesson learned from , after that, forget it and move on to the next challenge.
Costs are not causes; costs come from causes–––Deming
Fix the problem not the blame–––Deming
So what is the problem? Who is to blame? What costs need fixing?
American leaders/executives have been paid handsomely to reduce headcount just prior to each quarter’s 10-Q’s, and 10K’s, becoming the “darlings” of Wall Street for taking such “difficult actions.”
Just how difficult is it to terminate thousands of employees jobs once each quarter, then once again each year? How difficult is it to choose to move millions of jobs off-shore to “improve profits” at the expense of quality, lead times, variability, etc.? How “difficult” is it to take in billions of dollars in profits, only to re-distribute 91% of it from 2003-2014 to stakeholders through either stock buy-backs or dividends?
Far less difficult than it is to take the time to understand appreciation for a system, knowledge of variation, theory of knowledge, and psychology.
While I wish there was a fundamental improvement in American leadership thinking, there is zero proof that this indeed has changed one iota from 1980, when Deming warned American leaders about the dire straights America would find herself in if her leaders continued to be the “Forces of Destruction” they have proven themselves to be time and time again.
Love your thinking and efforts to make a difference Mark, please keep up the important work.–––Colin
[…] back to the times when you were the one being pressured for results by a shortsighted boss. Why embrace accountability if it simply gives your boss an easy excuse to blame you? Why not pass the buck to other team members and screw them over if you are only going to be blamed […]
[…] results by a shortsighted boss. Why embrace accountability if it simply gives your boss 	…? Why not pass the buck to other […]