tl;dr: In this post, Mark delves into the detrimental effects of a punitive culture within healthcare, arguing for a shift towards a culture of helping. Citing examples and personal insights, he examines how a compassionate, collaborative environment can enhance patient care, employee morale, and systemic improvement.
People tend to want to blame individuals for mistakes. We want to “hold them accountable,” even if that's a polite way of saying “blame and punish.”
Healthcare organizations, being made up of people, also tend to blame individuals.
Punishment is a hard habit to break. But we must. Lucian Leape, MD, one of the leaders of the modern patient-safety movement, reinforced this notion in testimony to Congress, making a statement that applies to most workplaces:
“The single greatest impediment to error prevention in the medical industry is that we punish people for making mistakes.”
How many systemic mistakes can you find in this article from the Institute for Safe Medication Practices (ISMP)? I've linked to it below.
Patient Death Tied to Lack of Proper Escalation Process for Barcode Scanning Failures
“ISMP obtained a report that helped to detail system failures that contributed to this tragic medication error.”
If healthcare had a strong culture of asking for help and pointing out problems, as companies like Toyota Motor Corporation and those who practice Lean management do… the nurse would have asked for help.
The nurse would have gotten proper help.
The patient wouldn't have died.
Blaming the nurse is unjust and counterproductive.
Some of the Systemic Failures
Below, I'm quoting from the ISMP write-up… where it states the fact that a “nurse was involved” — but that doesn't mean the nurse should be blamed or punished.
The patient was mistakenly given NaturaLyte orally instead of Suprep.
“NaturaLyte, which is available in a large plastic container, had been left in the ICU by the dialysis team for a different patient who was undergoing hemodialysis about 3 days before this incident.”
Why was the NaturaLyte even there? Why had it been left behind?
“When it was time to administer the bowel prep, the nurse went to the medication area and saw two large plastic containers labeled NaturaLyte, containing a clear liquid. The nurse assumed these were similar to GOLYTELY…”
Yes, that was a bad assumption, but humans make bad assumptions all the time, especially when overly busy, fatigued, or distracted. It's also difficult to be on guard for a “wrong medication” that isn't even supposed to be there.
“[The] nurse [may have] thought NaturaLyte was a generic replacement for GoLYTELY” — the names are similar and this isn't uncommon in healthcare.
Critics and blamers would say, “The nurse should have just read the label.”
Well, the nurse did try to scan the barcode, following the correct process. However, “… the barcode may not be recognized by many barcode scanning systems since NaturaLyte is not a drug and the barcode does not contain a national drug code (NDC).” The scanning did not work.
This is where a properly functioning “andon” system (and culture) based on Lean and the Toyota Production System would be helpful. If there's a problem, raise the alert. Thinking, “This is odd” should lead to the activation of what some health systems would call a “patient safety alert” system. And a supervisor or manager should come immediately provide assistance to troubleshoot or correct the situation.
The nurse did contact the pharmacy for help.
“Rather than sending a new labeled medication (Suprep), or physically reviewing the product that would not scan, a pharmacist sent a patient label that contained a barcode through the tube system for the correct medication, Suprep.”
That's a major point of failure right there. I'm not blaming the pharmacist. Was the pharmacy overburdened and understaffed? Were they too busy to come look?
They sent the “correct” label to be placed on the wrong medication. The barcode scanning now “worked” but not in the intended protective manner.
“…the nurse scanned the patient's armband, scanned the label provided by pharmacy, and administered about 240 mL of the NaturaLyte in its concentrated form. The patient began to drink the liquid but could not tolerate it all due to the bad taste and became nauseous.”
That's another red flag that should have led to the activation of a proper “andon” type system — and the response of a manager or the pharmacy to physical go and see the situation.
“…the nurse notified the physician.”
But the physician (who probably also wasn't there at the bedside) said to administer the rest of the wrong medication via a feeding tube.
There are now many people involved in this systemic error. Choosing to blame and punish ALL of them wouldn't help any more than finding one of them to scapegoat.
Another thing that screams “systemic error” was another nurse then making the same mistake.
“Another nurse (on the next shift) administered the rest of the concentrated NaturaLyte liquid through the feeding tube. The second nurse also thought that Suprep was similar to GoLYTELY, and was substituted with NaturaLyte. A physician who later assessed the condition as the patient deteriorated, also thought the container looked like GoLYTELY.”
Then the worst happened:
“Later, an electrocardiogram (EKG) revealed significant changes and the patient died the following morning. The cause of death was not mentioned in the report.”
Other Systemic Factors
As the ISMP points out:
- Some ICU nurses were pulled to other areas, therefore the ICU nurse had “two other high-acuity patients” — meaning they were caring for three patients instead of two
- The large plastic container prevented it from being send back to the pharmacy via the convenience of the tube system
- It's sadly common for dialysis products to be left behind in patient care areas — why hasn't healthcare learned from that risk (and what were likely to be previous incidents of this same type)?
ISMP Recommendations
They focus on the need for systems:
“…it is important to have processes in place to prevent these types of errors.”
This includes scanning original manufacturer barcodes and not a label added by the pharmacy, which can lead to a “false positive” scan — the correct scan of the wrong label.
“Also, develop an escalation process for what to do when a medication barcode will not scan.”
That's the andon process that I'm referring to.
“When a barcode will not scan, pharmacists need to visually verify that the medication matches what is ordered for the patient. It is not safe to send a label by itself. Labels must be considered part of the dispensing process and should only be placed on products by pharmacy personnel.”
The ISMP also writes about the need for staff education and communication. That's fine, but you can't rely on that alone. You need better systems and processes if you want to prevent mistakes and harm.
And, yes, unfamililar or unusual medications shouldn't be left behind — and if discovered, they should be removed.
Stop the Blame Game
How can we encourage or ensure that EVERY hospital learns from these mistakes?? How do we shift from a culture of punishment to a culture of learning, improvement, and prevention?
The headlines often, sadly, focus on the “tip of the spear” or the nurse who gave the wrong medication. It was actually NURSES, plural. And don't forget that there were many other people involved:
- The person or people who left the NaturaLyte behind
- Those who made the decision to understaff / overwork the ICU nurses
- The physican who was called
- Pharmacy staff, including a pharmacist
- The nurses who gave the wrong medication
A typical headline, this time from Becker's Hospital Review:
Kentucky nurse involved in drug mix-up that led to patient death: Report
The first sentence of the article gets to the more important point:
“A series of missteps led to a nurse inadvertently administering the wrong medication to a patient last summer at CHI Saint Joseph Health Main in Lexington, Ky.”
The problem wasn't a “bad nurse,” it was “a series of missteps.” They didn't have room to say that in the headline?
It sounds like the hospital, thankfully, didn't go down the punitive path:
“Kelly Jenkins, executive director of the state's nursing board, told LEX 18 there were “multiple process failures” that led to the medication mixup and that the nurse involved was not disciplined because of missteps unrelated to her role. The Kentucky Board of Pharmacy is also investigating the incident.”
But again, I thought the ISMP said it was “the nurses involved.” Not just one. Being involved doesn't mean you're responsible for it.
This headline is better in that it describes the systemic “mixup” better:
Medication mix-up blamed for death of a patient at Lexington hospital
Shame on Becker's for blaming a nurse in their headline.
——
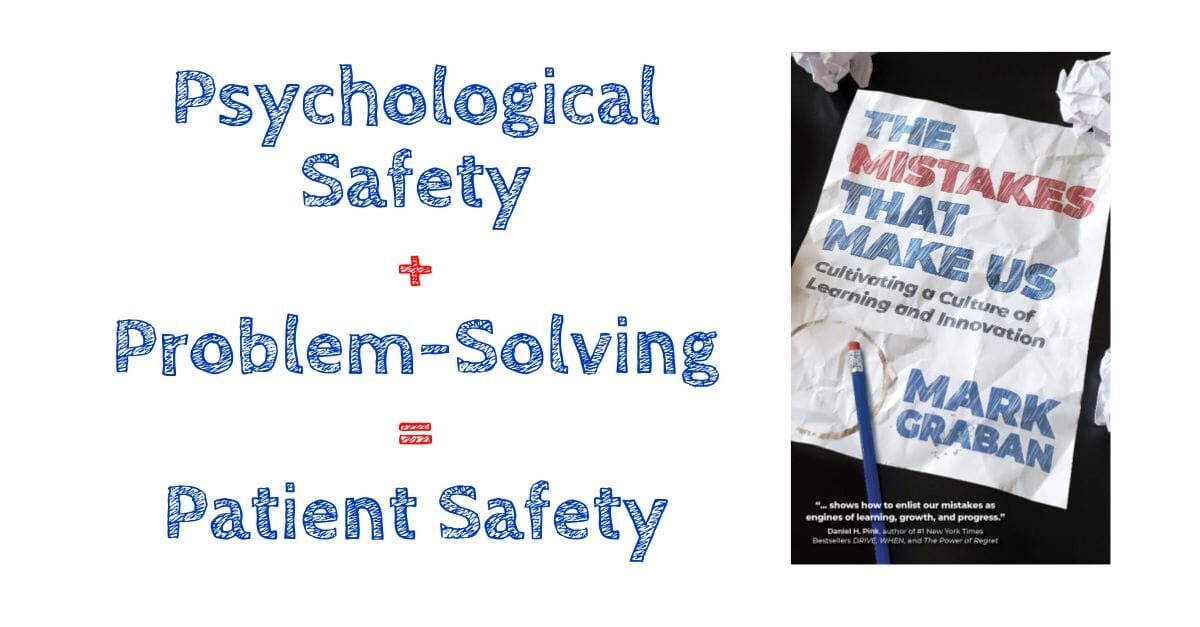
This post included an excerpt from my book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation — please learn more and consider buying the book via my website, Amazon, or other retailers in paperback, hardcover, Kindle, or audiobook formats. It's available now through Apple Books and coming soon to other eBook platforms.
Website –> https://mistakesbook.com/
——
We need both psychological safety and problem-solving if we're going to have patient safety.
If you'd like to read more about learning from mistakes, please follow me on LinkedIn, Mark Graban.
You can join the original conversation there on LinkedIn or post a comment below here on the blog.

Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s build a culture of continuous improvement and psychological safety—together. If you're a leader aiming for lasting change (not just more projects), I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s talk.
Join me for a Lean Healthcare Accelerator Trip to Japan! Learn More









