We're coming up on the 10th anniversary of the publication of the book that I co-authored with Joe Swartz called Healthcare Kaizen: Engaging Front-Line Staff in Sustainable Continuous Improvements.
I'll share more reflections about the book, what we would have done differently, and what we've learned since.
Today, I'm sharing an article that I wrote, originally published ten years ago by Texas Healthcare News (and I don't think it's online anymore… until now).
The Article
Kaizen. It is a strange-looking word. It might seem a little difficult to pronounce. Said out loud, it sounds a lot like “try-zen,” and we can equate the word with making things more zen-like in the healthcare workplace. Kaizen is a Japanese word that means “good change” or “change for the better.” Kaizen, as a management concept, leads to a calmer, better organized, more productive workplace where healthcare professionals provide improved patient care.
Shortly after Masaaki Imai introduced the principles in this 1986 book “KAIZEN,” Dr. Don Berwick published a piece in the New England Journal of Medicine promoting these principles, citing Imai, and defining Kaizen as “the continuous search for opportunities for all processes to get better.” But, more than 20 years later, it's easier for a health system to say they want a “culture of continuous improvement” than it is for them to make this a reality.
Suggestion boxes, committees, and endless meetings are not the path to continuous improvement. The Kaizen model is not very complicated – it is just different than the methods that health systems have tried in recent decades. What should be familiar, however, to healthcare professionals is that the Kaizen model utilizes the scientific method – in particular, the “Deming Cycle” of Plan-Do-Study-Adjust.
The basic Kaizen model has five steps:
1) Find
Staff and managers work together to identify waste or problems that interfere with providing ideal care. They can also identify opportunities that reduce frustrations for staff or provide a better patient experience. In the Kaizen model, no idea is too small to be worked on, as we see that lots of little small improvements add up to make a big impact. My Healthcare Kaizenco-author's organization, Franciscan St. Francis Health (Indianapolis) implemented more than 4,000 improvements in 2011 alone.
2) Discuss
Kaizen is not a solo activity. When an employee has an idea, they should have a discussion with their supervisor and, more often than not, with their co-workers. The manager's role is not to simply approve or reject each idea, as might happen in a typical suggestion box process. Rather, the manager serves a coach and collaborator, asking questions and making sure the idea is neither suboptimizing nor creates any risks or problems. The back and forth often leads to a better idea than the one that was originally suggested.
3) Implement
Even if potentially applicable to the entire organization, Kaizen ideas are put in place using small tests of change using the PDSA model. Rather than just assuming all changes are improvements, we test the change for hours or days, looking at data where we can to rationally evaluate the results. If we do not get the results we expected, or if there are unintended side effects, we can learn from that (instead of viewing this as a failure) and go back to the drawing board. If we do get our expected positive results, then we can spread that improvement.
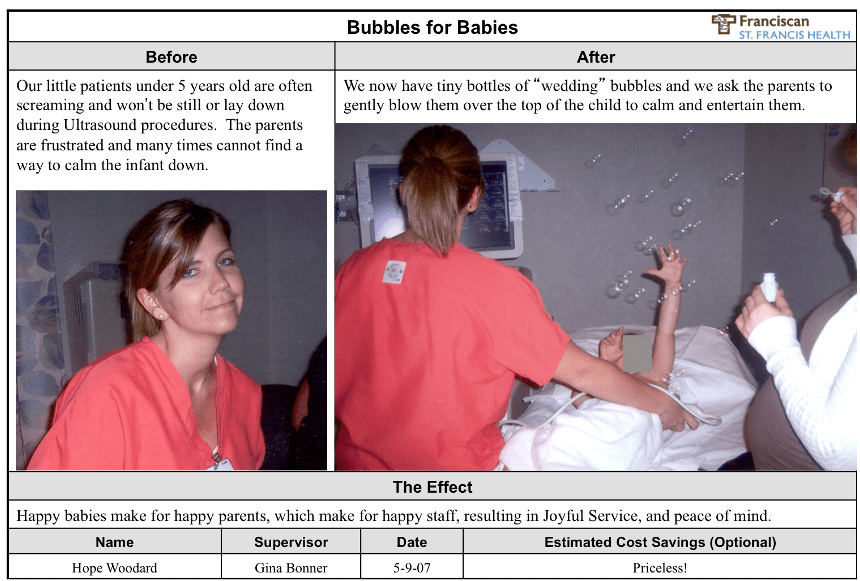
4) Document
It's tempting to skip this step, but doing a simple write up of each completed Kaizen can allow for reflection about the change (what did we learn?) and recognition for those involved. An example from Franciscan St. Francis is pictured here. As with many small Kaizens, it is difficult to calculate a specific Return on Investment (ROI) for each and every improvement. The benefits to patients, in terms of clinical outcomes and their experience, and to staff are indeed priceless.
5) Share
Documented ideas then get shared via:
- Department bulletin boards
- Hospital-wide display boards in public areas
- Home-grown databases (as done at Franciscan St. Francis)
- Commercial web software (like KaiNexus)
As this sharing occurs, ideas tend to spread naturally through the organization as they are adopted by others. Note this is different than a “roll out” where ideas are forced upon others who are forced to comply. In the Kaizen approach, we share improvements in a way that engages others without stifling their creativity.
This Kaizen style of improvement does require a different leadership model. Instead of being “the boss” who makes every decision, managers are coaches, facilitators, and partners in improvement. At Franciscan St. Francis, the CEO and COO are supportive of this culture change – and this has led to millions in direct financial benefit over the past five years. That's in addition to improvements to quality, safety, service, and morale that are more difficult to measure. Kaizen works in healthcare – for the benefit of all involved.
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation:










