When I blogged a summary of my recent Brazil trip, I said I'd write more about my visit to a hospital… so here's that post.
Thanks again to my hosts, Gemba Group, the consulting and training firm that has been helping the hospital that I visited — Hospital Mackenzie in Curitiba, Brazil. Specifically, this was the Evangelical University Hospital, a large 600-bed academic hospital (one of the largest in the city). The Mackenzie name was relatively new, as the result of a merger of hospitals. I was told that one requirement of the merger was that the combined hospital would pursue Lean.
Two of my hosts were the two people who are leading the Lean efforts — a physician and an engineer. The physician is based in Sao Paolo and he works with a number of hospitals, and I think that's also true of the engineer. The engineer and I had a chance to speak 1×1 and his background, like mine, is originally manufacturing.
I also got to meet the “administrative director” of the hospital (the CEO, in U.S. terms).
Here is a group photo from the end of our visit, with some process maps and a VSM in the background:

Emergency Patient Flow Improvement
The hospital is working on what some might call “Emergency Department patient flow,” but it's really a broader, extended “value stream” that goes across many departments.
The doctor told me he had read my book Lean Hospitals (which is available in Portuguese), which I appreciate. I think a bigger influence on their improvement work was the doctor traveling to the U.S. to take a workshop on E.D. improvement from Dr. Jody Crane and Chuck Noon, Ph.D. (another doctor/engineer pairing). Listen to my podcast with Jody and Chuck.
We had a chance to walk through their newly constructed E.D., which had opened just a month prior. They had implemented (and built space around) the “split flow” or “fast track” model that they learned from Crane and Noon. In this model, high acuity patients are sent down one flow and low acuity patients go down a separate flow. This improves flow for both tracks. Low acuity patients can be kept more vertical, or in reclining chairs, instead of beds, for example.
One physical improvement they made was reducing the distance and time it takes to transport a patient from the E.D. to radiology. This change was informed by Lean principles and their “spaghetti diagram” of the old space, as shown below:
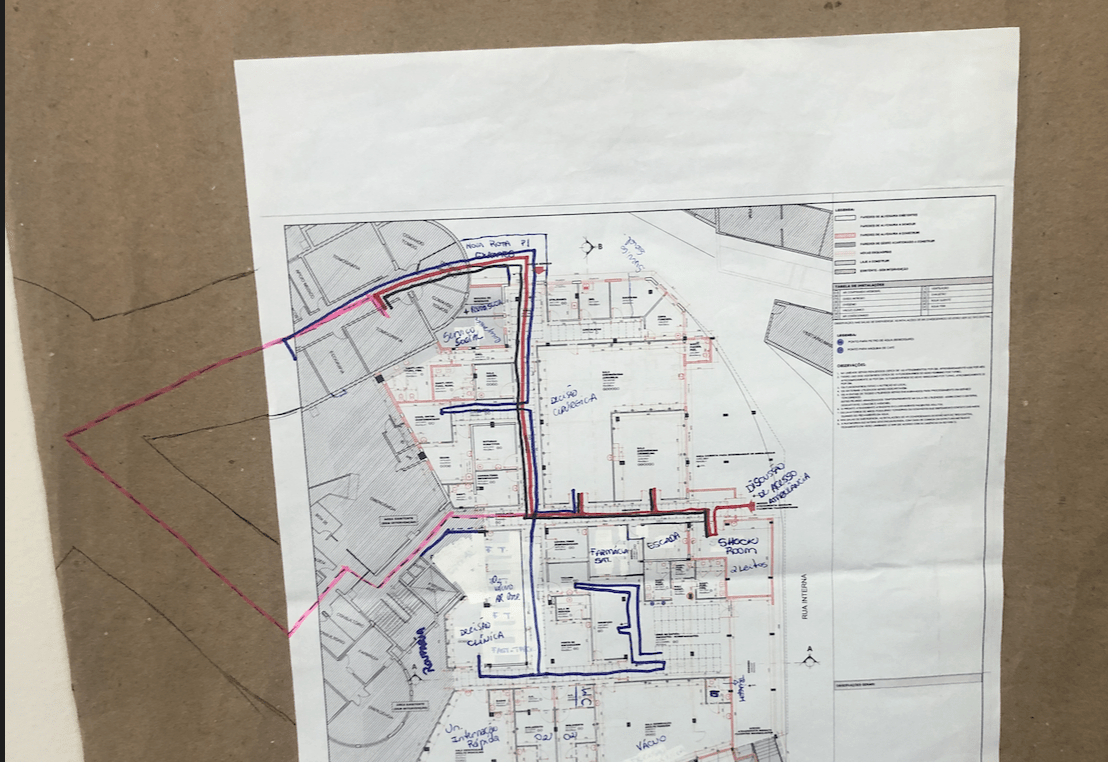
They knocked out a wall and created a corridor that goes straight through instead of going out and around one of two directions.
The hospital also implemented a patient tracking board and there was a new TV display that showed patients and their length of stay. Patients were color coded into green/yellow/red categories and that form of visual management helped them make decisions. For example, they used to send patients to x-ray on a First-In-First-Out basis, but now they prioritize based on flow and the time spent waiting, in addition to clinical priorities. They said the board helps with flow and visibility, as they can “now see priorities and length of stay” at a glance.
They realize they need to improve across the extended value stream, which leads to their huddles.
One other thing to note: the waiting room used to be “much bigger” and it doesn't need to be as big with the new flow and process. Waiting times are down, as well.
Daily Huddles
I was also able to observe a huddle, one of three that takes place each day with leaders from various areas — Lab, x-ray, E.D., pharmacy, etc. It's great to see that level of cross-functional communication and problem solving.
A nurse leader led the huddle, which was a standup meeting near the E.D. She was using a standardized checklist on a clipboard. They celebrated some successes in getting patients discharged. She asked if there were any dischargeable patients who had social assistance needs.
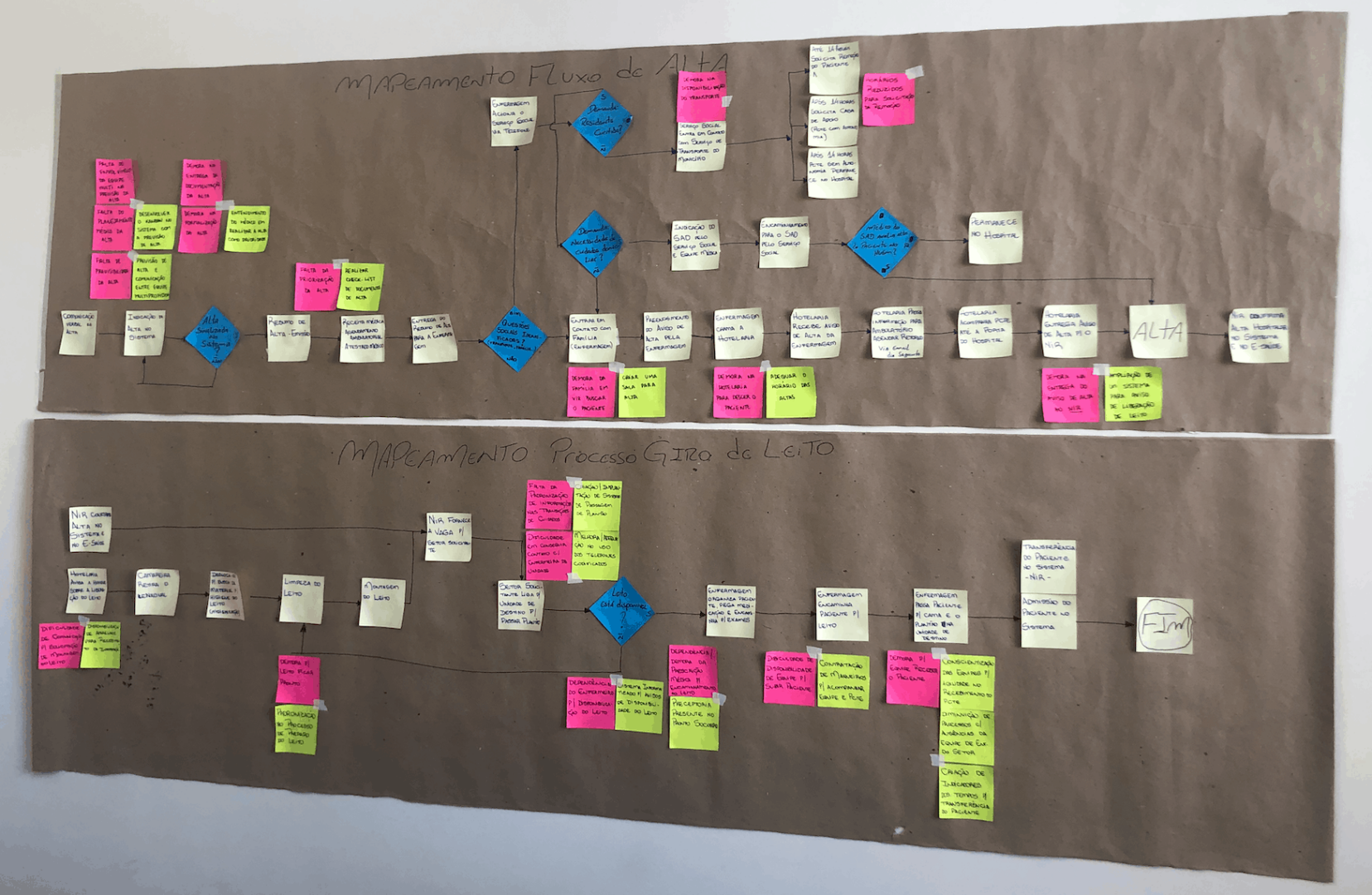
Discharge is one of the processes they had mapped out in the name of improvement (as also shown below). They are also working to better forecast patient discharges, planning home care and other needs earlier in the patient's stay (as to prevent delays at discharge). They've also mapped the bed turnover process to help improve that.
They also discussed a problem with lab results being slow that day, since it was affecting E.D. patient flow. There are separate Lean improvement efforts taking place in the lab.
At the end of the 10-minute standup huddle, the administrative leaders would bring lessons learned back and use that to plan the next huddle.
I asked what the benefits of the huddles were and was told they had “faster problem solving and faster decision making.” The “improvement of communication amongst the leaders” was described as “unbelievable.”
They also include environmental services and other support departments in the huddle. “They feel more a part of the hospital” and they better realize “their importance in helping save lives” and “not just cleaning floors.”
They added that “invisible work now seems more important” and that “everyone is a caregiver” (which is terminology they use at Cleveland Clinic, too).
Their Lean Overview
The lead physician shared a presentation about their Lean journey — at this hospital and at others.
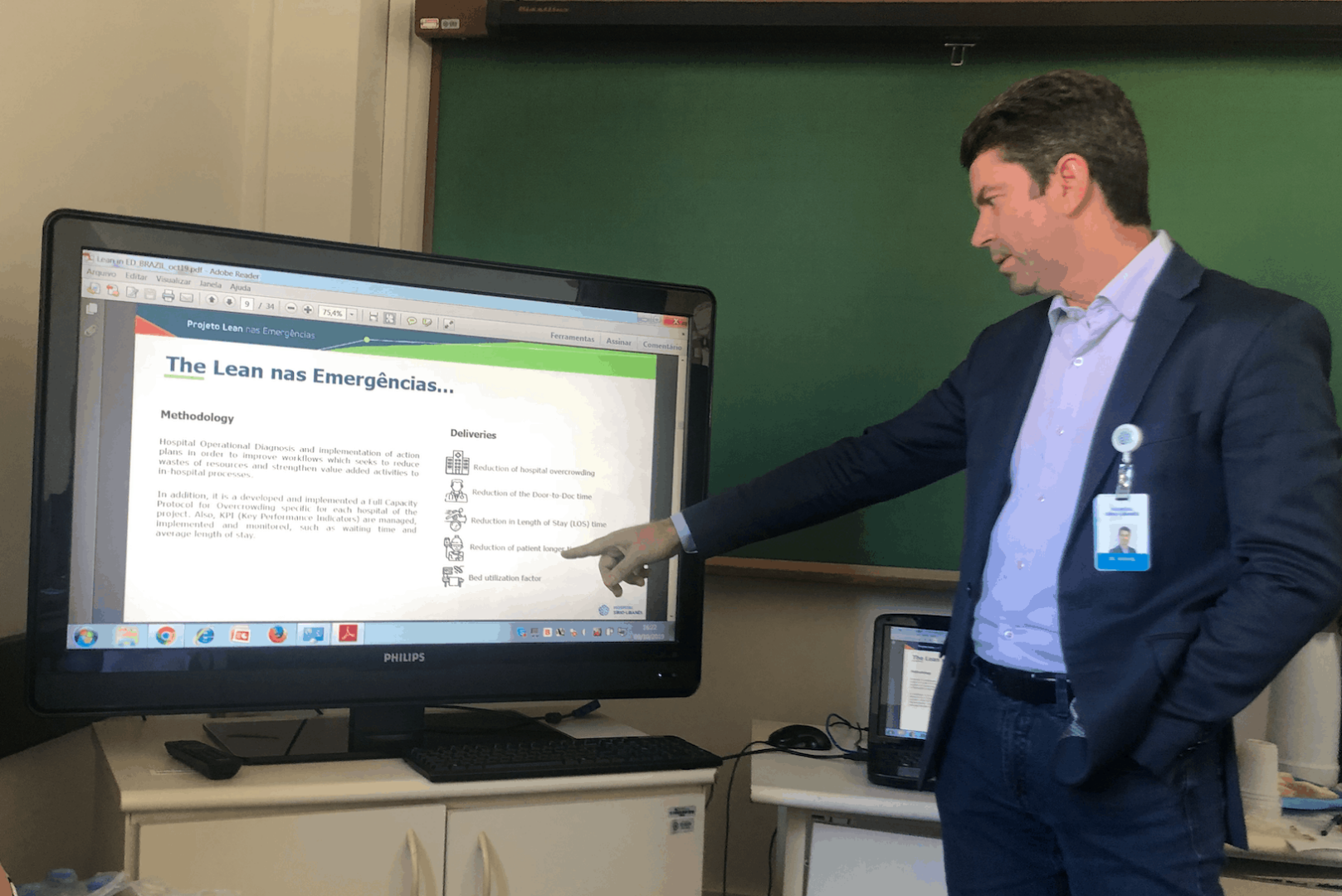
There has been grant funding to help improve hospitals through Lean.
Their focus is:
- Waiting
- Flow
- Quality
- Mistakes
Each hospital has a diad of a physician and a Lean specialist. Currently, this Lean E.D. improvement work has taken place (or is underway) at 57 public hospitals across 20 states in Brazil.
They are working to shift from tools to a culture and philosophy. They're incorporating change management and Kaizen-style improvements in addition to the large projects.
“You can't force people to change.”
Amen to that!
In the past, patients in the hallways (waiting for inpatient beds) “was seen as normal” but they worked to “define a new normal.” You have to start with a belief (what's possible?) and have leadership to help make it happen.
Thanks again to Gemba Group and Hospital Mackenzie for hosting me and allowing me to see and learn. It's very inspiring!
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation:










Looks like a great start. Was there much talk regarding of sustainability, or too soon in the process? Also, where did the duo pairing idea originate for them? Thanks for the insights.
Good question. I might be too early to say. But I do think their wisdom about not forcing change on people bodes well for their sustainability. Turning this into a daily management system and not just a project is also encouraging. Getting results that matter and not just training people is another good sign.
Very interesting article, it is great to see the progress that the hospital is making. I am a firm believer in the “daily huddles” concept, and was able to see how that idea was very beneficial in the company that I worked at. Bringing everyone together creates an atmosphere of collaboration, and brainstorming that can help with the problem-solving process. I have not thought much about flows in a hospital, and how efficient they have to be so your article gave me a lot of new knowledge. Thank you for sharing!
Love the insight! As a student at the University of Rhode Island pursuing a degree in Supply Chain Management, and soon a job in the health care/medical device field, I found this article to be very interesting and eye catching. I never knew about the capabilities and benefits lean six sigma would have in the hospital environment, but can now see myself enacting this positive change and these improvements myself. Lean is an extremely important tool, especially in hospitals the slightest improvement could save a life. Have you noticed any patterns or recurring problems hospitals are facing? What made you want to work in both the hospital/health care and lean space? Thank you for the great information!
Thanks for commenting, Matthew. I’m glad you’re interested in a career in healthcare. There’s still so much improvement opportunity. For now, I can answer the question about how I started working in healthcare by adding a link to this blog post:
https://www.leanblog.org/2017/05/reader-question-got-lean-healthcare/
Yes… and many of these problems are global problems. Patient safety, quality, patient flow and access, cost, staff satisfaction, and more… I also write about that in Chapter 1 of “Lean Hospitals,” which can be found also in the link I posted above.