My blogging and other typing might be limited a bit since I had a minor outpatient procedure to remove a ganglion cyst (or something similar) from a knuckle on my
In December, I noticed a growth on a knuckle. It felt like a cyst that was filled with fluid. My finger is pretty mangled from a high school baseball injury that never healed properly. But this cyst caused more discomfort and pain in daily life — when typing or, worse, when banging it into something.
Here is the cyst:

In late January, I finally said something about it to my primary care doctor, when in for a routine checkup. He said he could drain it, but it would likely come back. I'm more of a root-cause solution kind of guy, so he referred me to an orthopedic specialist. It seemed quite likely, from Dr. Google and my real doctor, that it was a Ganglion cyst that could be removed surgically… getting more to the root of the matter in a way that would prevent it from coming back (no guarantees).
I was able to get an appointment pretty quickly – on February 7 (or that was the first day that worked for me). The orthopod looked at my finger and after about two seconds confirmed that it was what I thought it was – a Ganglion cyst… and we could get it scheduled for removal, which would require a trip to an outpatient surgical center.
The orthopod's clinic had a sign that seemed to invite feedback (or maybe they were conditioning me to give top marks on any patient satisfaction survey).
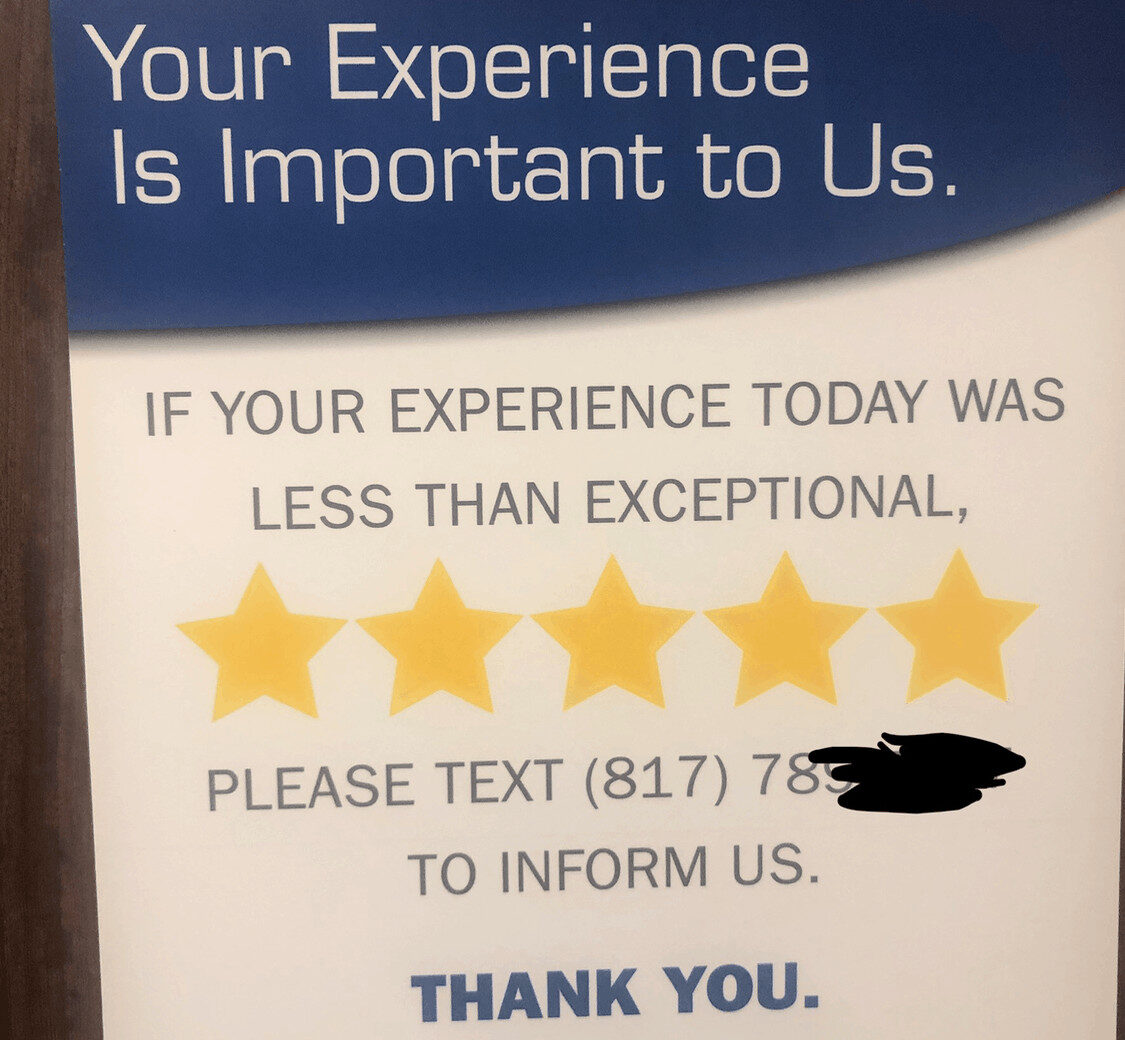
I guess it's nice that they seem to want feedback. But one thing that's puzzled me about healthcare is why they don't take advantage of having the customer (the patient) actually being right there, as I've blogged about before:
This other poster in the room made me feel confident that the medical team knew the names and locations of major body parts:

I texted to let them know (as I blogged about) that their confirmation text message gave the address for the wrong clinic.
I did get a response pretty quickly and I hope they fixed the root of the issue:
She was able to get me scheduled for surgery on March 1st, but March 8th worked better for
As I left, I thought it was funny that the huge sign over the exit door apparently wasn't effective, so they added a paper sign:

Yay,
Weeks Before the Procedure
I was called around February 5 or 8 to talk about payment for the procedure. I was given an estimate (about $3000 total since my wife and I haven't yet met the deductible for her health insurance). I was asked if I'd like to pay now (in advance) or before the procedure.
Um, I understand the time value of money, so I chose to pay the morning of the procedure, thank you. I can't fault them for trying, LOL.
Days Before the Procedure
Again, the procedure was going to be March 8th. I came down with a fever and cough that I was battling from February 27th through March 5th. I ended up on an antibiotic.
So, I called the surgeon's office on March 5th to make sure that having been sick wasn't going to cause any problems. I left a voice mail. I don't think this led to a call back.
On the 6th, I received an email that talked about prep for the procedure. During the February 7th consult, the surgeon and I agreed that this quick procedure could be done with just local numbing. There was no need for sedation or anesthesia.
I was told they couldn't give me the scheduled time until the day before:
1. Please arrive… approximately 1 to 1.5 hours prior to your surgery time. You will be notified of your arrival time the day before your surgery (between the hours of 3:00 pm and 6:00 pm). Upon arrival, please notify the reception desk staff.
I was told I could drive myself home, but my wife was going to arrange to come with me and we both would have appreciated more notice in planning our day.
I was perplexed by this instruction would come just TWO days before the procedure:
“4. STOP all BLOOD THINNERS (for
example: Coumadin, Plavix, Lovenox, Motrin, Advil, ibuprofen, Aleve, Naprosyn, aspirin, Vit E, or fish oil) for seven (7) to ten (10) days prior to your surgery, unless otherwise instructed by your physician. You may use Tylenol based products. Additionally, refrain from herbal and/or prescription or OTC diet medications for seven (7) to ten (10) days prior to your surgery.”
I'm not on blood thinners. But I am on one ongoing prescription medication. Did they really want me to stop taking medications “7 to 10 days” prior to surgery? Is it 7 or 10? 8.5?
Why would you send this out just TWO days in advance? Does this lead to canceled procedures? They certainly asked me to PAY many weeks in advance. Why wasn't this automated form email sent sooner?
I had been on Ibuprofen and Aleve due to my fever… did that mean I had to postpone my procedure?
I called to get clarification and was told, “Oh you can ignore those instructions since you're not being sedated for a ‘minor procedure'.” They can't have a separate set of instructions for minor procedures? Do they have to send the same generic email to all patients? Is this “patient-centered care?”
The generic email said I couldn't drive — except the surgeon said I could:
3. You will not be allowed to drive for at least 24 hours following your procedure; therefore, you will need a responsible adult (over the age of 18) to drive you home. We ask your responsible party to remain at the surgery center during your stay with us to allow your physician to provide instructions and information regarding your procedure and post-operative care. Taxi, Uber or Lyft transportation is NOT permitted unless you are accompanied by a responsible adult. Furthermore, you should have someone stay with you for 24 hours after surgery.
But the email ends with:
“We believe in excellent care!”
Easier said than done?
I got a confirmation call the day before and was told, again, that I needed to fast. “No, I'm not being sedated,” I said. “Oh, OK, you can eat then,” I was told.
The Day of the Procedure
Oh, I was called late on Thursday and was told to arrive at 10:15 AM. I was told my procedure would probably be at 11:45 AM, but they might be running ahead of schedule.
I was checked in by a friendly staff member. They collected my payment, and told me to go sit in the waiting room.
They had guest wi-fi, but I had to go ask the woman at the front desk what the password is. I wonder how many times a day that happens… they could just post a sign with the password (eve the American Airline Admirals Club does that).
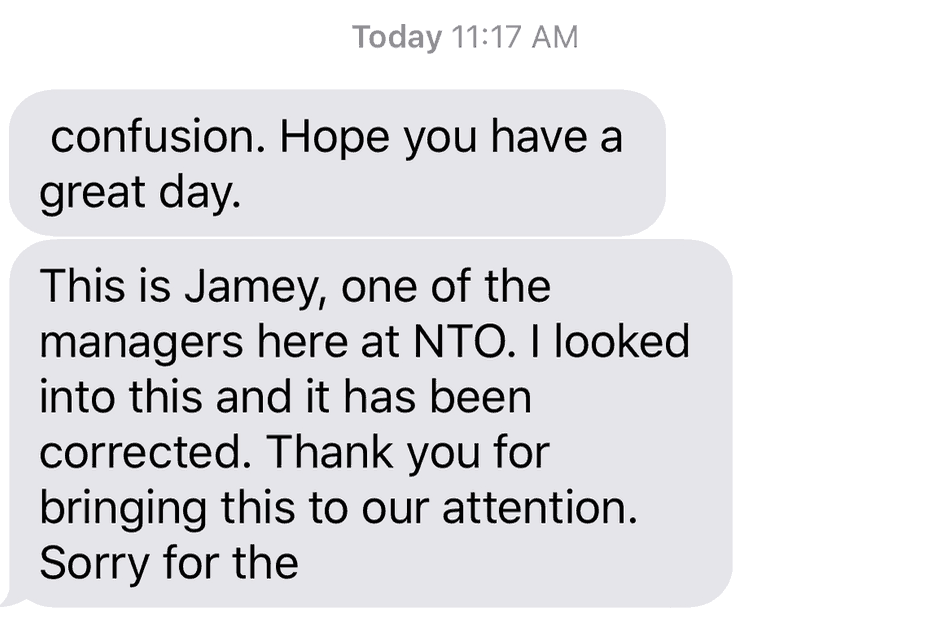
This sign was posted in the lobby. It was a generic sign that, again, didn't apply to me. So, I made some tea from their machine. They could add “if being sedated” to the sign.
I could see the digital patient flow status board in the lobby. At about 11 AM, I could see that one patient was in the OR with my surgeon and two more appeared to be waiting in front of me. It didn't seem like 11:45 AM was likely.
Now, to be clear, falling behind schedule was the LEAST of my annoyances. Safety and quality come first. I'd rather wait than have the surgeon rush through anybody's case.
That said, I did tweet:
Right now I accept my fate as “inventory.” I am sitting here to further the goal of maximizing surgeon productivity. I don't want the surgeon rushing to stay on schedule for me or anyone else. Safety and quality first.
I also noticed, between the waiting room bathroom signs and the pain killer I had been prescribed (just in case) had language that wasn't as clear as possible:
There is a lack of clear simple language. Prescription bottle says to take pill “by oral route” instead of “by mouth.” Is there a question about a pill anyway? Sign on bathroom door talks about “voiding” instead of “urinating.”
I got called back to pre-op prep at 11:47 AM.
The nurse was
As she was prepping me, she was distracted by her smart phone, which had some app showing the live status of her son's high school baseball game (he was out of school playing some tournament). I'm not sure if I should have been bothered by not being the sole focus of her attention.
I was given socks to wear that are quite literally tube socks. They're not shaped like a normal sock we'd normally wear. Is this cheaper? It sure wasn't more comfortable. Why is there non-slip tread on the top of the sock? Doesn't that add cost?

I guess they worked. Sort of.

So, I sat for a while in the pre-op bay. Thankfully, nobody tried putting an IV in my arm, although a few people still thought I was going to get one.
In healthcare, people say things like, “We're not just making widgets.” Well, a good Lean factory has “a plan for every part” and I'm not sure this surgical center had a good plan for me. It felt like constant chaos and confusion.
As she was filling out more paperwork, the nurse noticed and commenting that she has been writing 2018 as the year on all forms today. Ah, that pesky problem known as human error. Maybe they could post a sign above the patient's head reminding people of the year.
If that sounds silly, they do post a picture of a cartoon frog reminding people to use hand sanitizer (which I don't recall seeing used even though another sign, in red, told people to).
The nurse said:
“The paperwork is going to take longer than your procedure.”
That seemed accurate, considering the paperwork before and after the procedure.
I was asked to sign my “John Henry” on the forms, which sounds like a cheap knockoff of a “John Hancock” signature.
The surgeon came in and asked if I was going to be sedated. Nope. I'm fine with local, right? She seemed sort of convinced.
She confirmed my name and procedure (as did everybody else) and she marked the correct finger and signed her initials:

About 1 PM, I was wheeled back to the operating room. Before I went, there was a bit of confusion, again, about the planned Lidocaine injection.
The surgeon gave verbal instructions to the nurses: “He gets 5 [mg?] and she [pointed to another patient] gets 20.”
Is that really how the instruction is given? I was hoping somebody didn't mix that up.
As I was being moved, the nurses were again confused about WHERE the injection would occur – before I was moved or in the O.R.
I was brought into the O.R. I got moved to the table and the setup was taking place. I was asked if I had a preference for the music that was played. I said no and deferred to what made the surgeon comfortable and happy.
So, that was
It was interesting being awake during the procedure, which only took about ten minutes. The worst discomfort was the Lidocaine injection, just like at the dentist.
Everything seemed to be a success. They gave me a choice of pink or blue tape (why make assumptions in this day and age, I guess?):
There was more paperwork. It was probably a good thing that I didn't need sedation, because I was brought back to the pre-op nurse who informed me, “PACU is full” (Post Anesthesia Care Unit). I wonder what care I would have gotten if I had been sedated?
The nurse escorted my wife out of the surgical recovery / prep area and had the manager keep watch over me (which might not have been necessary since I wasn't recovering from sedation). The manager gave a nod from down the hallway, but never came to ask how I was doing. She especially didn't ask if I had any concerns or feedback.
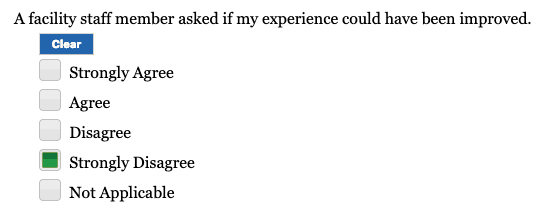
The survey I was emailed on Monday morning implied somebody should have asked for such feedback:
I was given a generic thank you card that implies they care about continuous improvement:
We'll see if they care about feedback.
I was also told that I would get a call “tomorrow” to see how I was doing. I think that was the fifth time that somebody asked me for my cell phone number that day.
I did not get a call.
As I tweeted about this, a few people asked, “Are you sure you trust them to do the surgery?”
So, at what point do you begin questioning the competency of the folks about to perform surgery on you? You are going in for complete amputation of your left lower leg, right? Or was it your right big toe…
— Karen Skinner (@KarenSkinner) March 8, 2019
I wasn't thrilled with the process issues. But would another surgery center have been better? Was it worth delaying my procedure over? No.
Are there things that could be done better? Yes. Will they improve? Who knows.
My main piece of feedback is about the timing of the pre-op instructions. They need to send those out at least ten days in advance so patients can confer with their primary care docs or other specialists, if needed.
I think I've survived this. I'm working on not getting an infection. Thanks to those who tweeted best wishes…
Other Tweets and Social Responses
Mark, You are just like me with the curse to constantly evaluate processes and look for the stupid way processes are designed. It is frustrating. My wife has been with me for over 30 years and has the curse too.
— John Dyer (@JohnDyerPI) March 8, 2019
The thing is… I can't help an organization that doesn't necessarily want help. I also didn't leave unwelcome books behind:
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s build a culture of continuous improvement and psychological safety—together. If you're a leader aiming for lasting change (not just more projects), I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s talk.
Join me for a Lean Healthcare Accelerator Trip to Japan! Learn More










So I did get a follow up call today… but not as a result of me doing the survey online.
I think when they told me on Friday that they will call “tomorrow” — do they really mean “next business day?”
The woman who called asked if I had feedback and I limited what I told her to:
1) The timing of the pre-op instructions
2) The lack of a playbook for my case and confusion about them wanting to sedate me
I got the generic “I’ll pass that along” and “hopefully we’ll fix those issues for future patients” response.
I wouldn’t wager a large sum of money on things really getting fixed…
Funny, by chance this morning at the dentist, before I read your blog, the hygienist and I got to talking (hard to do during a cleaning) about spelling and a person who works at an orthopedic office with her mother, who asked “how do you spell ‘shoulder’?” She talked about this commercial that I later found, “with the guy having finger surgery” – I think it’s an oxygen monitor on his finger. Funny! But neither of us could remember what company the commercial was for – I came the closest, knowing it was a cell phone provider, even though I seldom watch TV.
Yeah, that’s a finger pulse oximeter for measuring oxygen saturation in the blood…
Excellent post as always Mark. I work for the NHS in the UK and make the exact same observations; not just as an Improvement Practitioner working within the system but as a patient and a taxpayer. If you were to see it yourself you would not be able to believe it! it is overwhelmingly frustrating at times!
Marco – It’s sad to see (and hear about) how common healthcare delivery and operations issues are across different countries. The insurance and payment systems might be different, but there seems to be waste everywhere.
I wonder if I would have been approved for this procedure by the NHS and, if so, how long I would have had to wait? I don’t ask this to slam the NHS… truly just curious.
Google tells me if it was just cosmetic and not causing impact on daily activities it is not likely to be approved, however this is dependant on local commissioning decisions. If it was approved I expect the wait for surgery would be around 5-6 months if you were lucky.
Thanks, Marco.
I’d say my cyst was not just a cosmetic issue. There was some pain and discomfort. Was it debilitating? No… could I have lived with it for a while? Sure.
Am I glad I got it removed? Yes… I did have to pay $3000 out of pocket to meet our health insurance deductible. In England, I might have waited, but it would be “free at the point of care,” right? Well, maybe I would pay for parking. I didn’t have to pay for parking here…
Was it worth $3000? Maybe… BTW, that was about $400 to the surgeon, and $2600 to the sugery center.
Thanks for sharing Mark. I am glad you are better. This experience reminds me how important it is for teams to truly observe what the customer goes through. We might watch a process and say it meets the right metrics but do we really have empathy for what customers are going through? The safety risks are also frightening especially when you think of people not savvy in healthcare could well be in danger.
The picture of the door is crazy. Is it really a staff entrance only door or is it for check-out? Maybe needs a third piece of paper saying what it is really for.
Thanks Brian. The finger is getting better… it only hurts when I bend it… and it doesn’t bend real well yet. I’m supposed to keep it mostly immobile and wrapped for a few more days.
The door photo was inadvertently misleading. The staff door sign is seen through the glass on the exit door. That’s another door you see through the door.
Great point about customer empathy and really understanding what people are experiencing. Are we concerned about the patient experience or just the patient survey metric?
I managed to develop a bit of a surgical site infection. Ugh. I got put on an antibiotic. I don’t know if that’s a process issue or a patient education issue or bad luck.
With the antibiotic and some steri-strips, the incision has really healed up nicely the past few days.
Comments are closed.