Mark's Note: Today's post is by my friend and Healthcare Kaizen co-author Joe Swartz.
Joe's Note: These comments are my own opinions and do not necessarily represent the views of Franciscan Health.
At Franciscan Health, we were struggling to create a system-wide standard for our improvement boards. Although we had deployed them to over 50 departments across our 14 hospitals, it has been a struggle to agree on what the boards should look like. Five of our hospitals used rows for each key metric while nine of our hospitals used columns for each key metric. However, now our leadership was asking us to become more standardized across our system.
Maturity Model
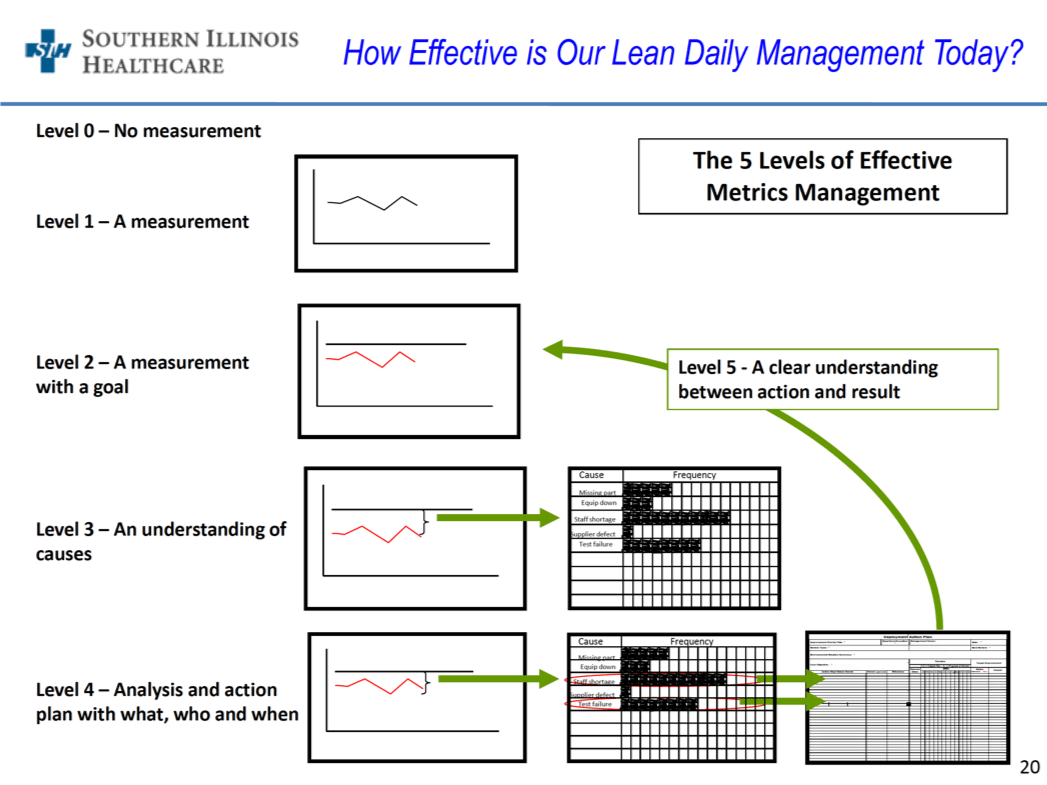
Then, as the old saying goes, “When the student is ready, the teacher will appear.” At a recent Catalysis-sponsored site visit, Jake Lingle, the System Director of Continuous Improvement at Southern Illinois Healthcare (SIH), presented a Lean Daily Management maturity model that has five levels of maturity.
The first level is simply picking one metric on which to focus and beginning to measure that.
Level two is setting goals for that measure.
Level three is an understanding of the causes of the gap between the current performance and the goal.
Level four is an analysis and action plan.
Level five is a clear understanding of what actions drove the improvement results.
See an illustration provided with SIH, shared with permission:
From this, I realized that the important thing is not the appearance of the boards.
What matters is how we use the boards and I now recognize that they will look different depending on the maturity of each department.
Content
At another Catalysis-sponsored site visit, Kevin Gazley of the Cleveland Clinic (see past blog posts about them) gave a presentation about their boards. He said that their biggest constraint was wall space in their already-crowded nursing units across their wide variety of hospitals. That constraint had forced them to have boards that look different. In some cases, everything was on one wall and, in other cases, the boards were broken up and spread across several partially-full walls. In other settings, they had no wall space, so they had to buy a self-standing board on wheels, using the front and back side of the board.
Some of the boards used rows for the metrics and some used columns, just like the variation in our boards at Franciscan Health. They also had problems getting agreement on a standard board. After much discussion, they decided to get a consensus on what functional components a leader should see on each of their boards.
The Intent
It was very helpful to see the approaches from SIH and the Cleveland Clinic. I wondered if our improvement team could agree on the intent of the boards. So, I asked our team members why we have boards and what we are trying to accomplish with them. After some thoughtful dialogue, we arrived at the following intent:
To create a cultural transformation of everyone engaged in continuous improvement, starting monthly or weekly, and driving over time toward daily.
As with the Cleveland Clinic, we began to understand the functional requirements of the design. We discussed what function the boards would need to enable based on our intent. We came up with the following list with almost no disagreement.
Requirements of Level Five Maturity Standard Boards – Rev 1
The improvement board system must enable:
- All employees to see the connection of system and facility goals to relevant unit or team goals – in order to focus at the Gemba on what is most important for our organization.
- A focus on the vital few metrics at any one point in time, especially early when the boards are not yet mature.
- Setting of Targets for key metrics.
- Tracking of key metrics over time (using methods such as run charts) to see if we are improving toward each target.
- Good problem solving
- A drill down into the potential causes to search for the root causes of problems (such as Pareto charts).
- Action plans for tests of change (i.e., Kaizens, PDSAs, A3s) – and test progress tracking, reflection & refinement, and connection to effects on metric performance.
- Improvement ideas being generally prioritized to SQDC (Safety, Quality, Delivery, Cost) and Effort vs. Impact.
- Gemba Walk communication with leadership about tests of change, reasons why, roadblocks to remove, and opportunities for spread.
- Visibility of patient feedback.
- Celebration of our good work, such that employees, leadership, and patients see the benefits of improvements.
As Simon Sinek says, “All organizations start with why, but only the great ones keep their why clear year after year.”
Just as form follows function, we needed to step back and understand the function of the boards. Our lesson is to dig deeper into our improvement work and ask fundamental questions such as, “Why are we doing what we are doing, what can we expect to change as we mature, and what are the functional requirements of the design?”
We recognize that we are on a learning journey and we do not suddenly have improvement boards that look the same across our system. However, we now have a rough agreement across our team about what we are trying to enable and to accomplish with the boards, and what should be on our fully-mature boards.
With agreement on the whys underlying our boards, we are one big step closer to having standard improvement boards.
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s work together to build a culture of continuous improvement and psychological safety. If you're a leader looking to create lasting change—not just projects—I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s start a conversation.








![When Was the Last Time a Leader Around You Admitted They Were Wrong? [Poll]](https://www.leanblog.org/wp-content/uploads/2025/07/Lean-Blog-Post-Cover-Image-2025-07-01T212509.843-100x75.jpg)