As I blogged about on Friday, I had two visits to the same dental practice last week… one very frustrating and the other one near perfect.
I added a comment to the post that elaborated a bit on some discussions with good Lean thinkers after the first visit.
As I wrote there (editing and elaborating below)…
A few people, including my future podcast guest, commented something to the effect of, “They need Lean!”
Do they? Do they NEED it?
Somebody made a similar comment on Twitter: “They need process improvement!”
Do they? Whatever we call it, does the business (the dental practice) NEED to improve?
Sadly, the answer might be “No. No, they don't need to improve.”
Is there room for improvement? Yes. Can they improve? Probably, if they really want to. Should they improve? That's up to them. Or the marketplace.
It seems that the process (including my waiting and non-value added time_ is fine, from their perspective. The practice seemed busy. They're in a good part of town with a well-insured population. The other clinic that operated a few miles way under that same umbrella brand name closed down, so some patients were shifted over there.
The owner of the dental practice might think their first priority is to keep everybody busy. That, of course, makes sense on one level, since you don't want to pay people to not work.
But, as an Industrial Engineer, I learned queuing theory and you quickly learn that when you have a system where the resources (machines or people) are fully utilized, the tradeoff is that the patients (or the products in a factory) will end up waiting. You'll have poor flow. There will be delays.
Everyone is busy, but the patient suffers.
Lean encourages us to focus on FLOW instead of full utilization. When patients flow better, they might be happier. You might get more referrals and more patients. So, you work to reduce waste and improve processes to further reduce delays, hence increasing capacity. This can be a more powerful virtuous cycle that offsets the “waste” of paying people to not be working 100%.
The other secret is that when the dentist or employees aren't doing value-adding work, they can use that time to work on process improvement.
As Toyota's legendary Taiichi Ohno said:
People don't go to Toyota to work, they go there to think.
Pushing Change Leads to Pushback (and That's Natural)
So, I could come marching in and say, “You need Lean,” but I'd be jumping to a solution. I wouldn't expect that to be well received, even if I gave them a copy of the book The Lean Dentist.
I could say, “You should consider Lean, as it would be greatly beneficial,” but I'd still be pushing. And they'd understandably push back. It's human nature.
This dynamic is one reason I've been learning about (and trying to practice) “Motivational Interviewing” as it relates to change management in the workplace and to personal change.
Instead of pushing answers at the dental practice, I'd do well to build a relationship and start on that conversation about change. It would be better for me to get the dental practice to articulate their goals, needs, and motivations.
If they are being “resistant to Lean” or “resistant to change,” I'd need to respect that “resistance” is a normal part of the change process. Change is a PROCESS. It takes time and conversation. Motivational Interviewing is about coaching, not commanding others to do something.
Pushing Change on the Patient
So, this made me think about the dental assistant's interactions with me.
They checked my gums and the pocket depths. It wasn't as bad as it has been before, but it wasn't great. I know that I should floss nightly, but I don't do that every single night. I brush my teeth without fail. That's important to me. I know why I should brush (there are many reasons) and I know why I should floss.
The dental assistant was kind, but she basically gave me a mini lecture about needing to floss more regularly.
Thinking about Motivational Interviewing in a clinical setting, the one lesson there is that it doesn't help when an expert tells you something you already know.
“You need to stop smoking.” The patient probably knows that.
“You should drink less.” The patient probably knows that's a good idea. They might even want to. But they don't drink less. They don't stop smoking.
People are complicated. Something can be rationally good for us and we still won't do it.
The past lectures from dentists or assistants about flossing aren't changing my behavior.
So that made me think of Motivational Interviewing.
The Motivational Interviewing Approach
She might have, instead, started by saying something like, “Can we talk about the health of your gums?”
Sure, I'd be open to that.
She might then evoke my own knowledge by asking, “Tell me what you know about flossing…”
I'd say, “I should floss every night… but I don't.”
The difference there is that I am the one articulating the need. That expresses at least some desire for change, as opposed to another patient who might say, “Flossing is a scam.” That's a different conversation.
The assistant might ask me, “Why is it important to you to floss more?”
I'd say things like, “My gums will stay healthier. I won't need as much treatment. That will save me time, money, and discomfort. I want to keep my teeth.” Things like that.
If she was evoking “change talk,” when that's powerful. Me speaking out loud is me convincing myself why I should do it.
After thinking about this a bit, I did a Google search and found information about applying M.I. to patients and flossing. There are even videos that show how this might go:
In this video, the hygienist goes into the “On a scale of 1 to 10, how important is it to you?” question that's used in M.I…. also asking the patient what would it take to move your number higher. That pair of question evokes change talk. She also asks the patient what she knows, a helpful method, as I said:
She asks the patient what steps she might take. She asks about her biggest challenges (a question that might evoke “sustain talk” instead of change talk). She then asks if it's OK to make a few suggestions (and the patient said it's OK). M.I. teaches experts they should always ask before telling (and not start telling right away).
Here's another, longer instructional video about M.I. in a different dental situation:
The dentist isn't just leading by asking open-ended questions, she's also using M.I. techniques of making affirmations and reflections — statements that move along the conversation about change.
That eight-minute discussion took longer, but would likely be more effective than a quick directive scolding about “don't smoke.”
Isn't the same thing true with change management in the workplace or Lean? “Go slow to go fast,” right? Pushing change might seem quicker, but it might also be what John Kotter calls the illusion of progress.
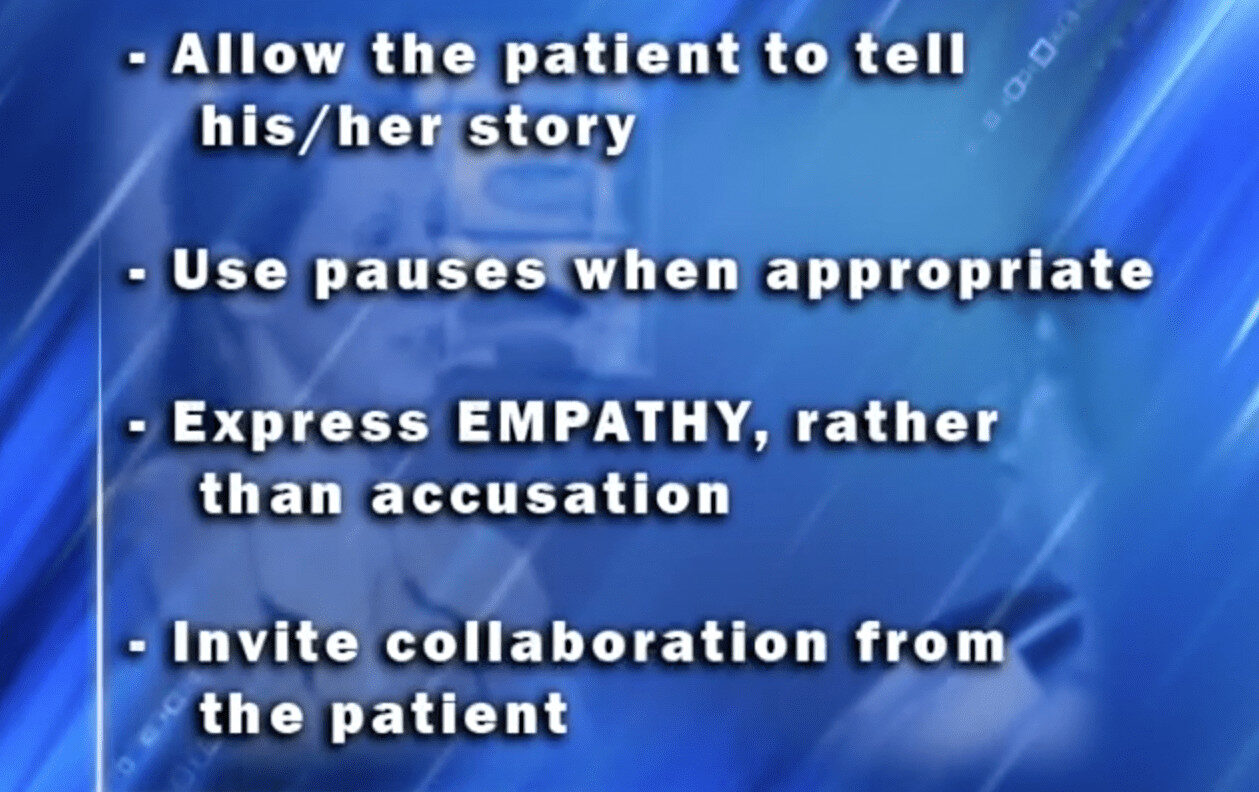
As the video summarizes, here's some of what the hygienist did well:
That's why I think these Motivational Interviewing methods and mindsets (which include respect for the patient and their choices) are powerful. What do you think?
Oh, and for contrast, here is the “non-Motivational Interviewing” version of that second discussion:
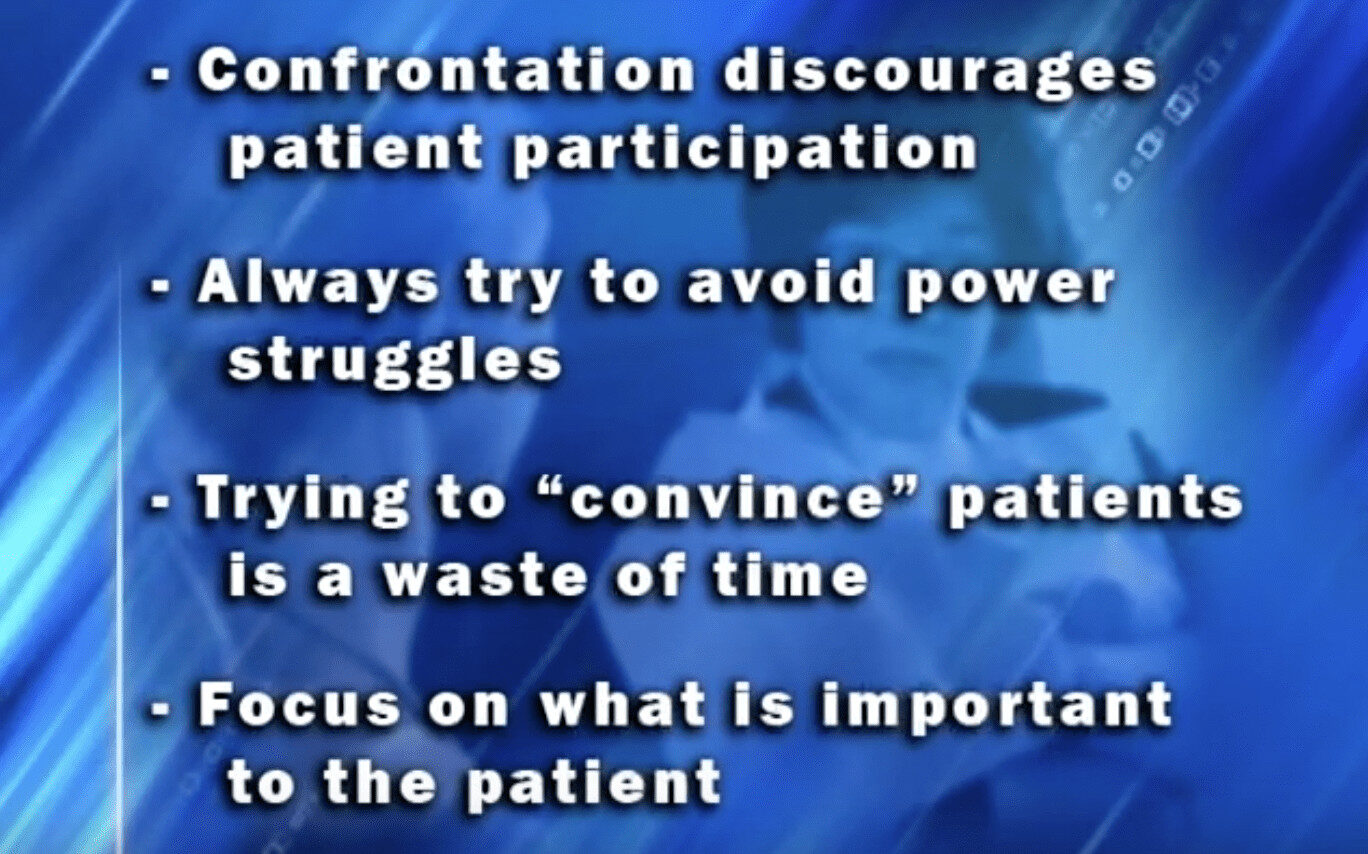
The summary of some of the behaviors that aren't generally successful, with patients or in the workplace:
How are you as a change agent or a Lean leader? What helpful or unhelpful behavior do you see from others?
Which version of that patient in those last two videos seems more likely to change?
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s work together to build a culture of continuous improvement and psychological safety. If you're a leader looking to create lasting change—not just projects—I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s start a conversation.










Mark, good post. The two videos and especially the second one mirror well what I learned the week before last at the Lean Coaching Summit in Seattle — open-ended questions, reflection statements. The second video reinforces these practices. Her reflection statements sound natural – not rigidly formatted as per MI guidelines. Thanks.