Toward the tail end of last week's Lean Healthcare Transformation Summit, I was having some symptoms that I equated with desert allergies. I'm talking about things like dust, with Palm Springs being an oasis in the desert, lest you think I'm allergic to dessert.
On the flight home, I was congested and my ears were painful on final approach. Saturday morning, my wife encouraged me to see a doctor. I tried one of the small clinics at a national pharmacy chain. As Edward Norton's character said in “Fight Club,” “it's a major one.” Readers probably realize it's one of two options, but I won't say which one or which city this was in. It doesn't matter. I'll just call them WalVS.
BUSINESS WOMAN
... Which... car company do you work for?
JACK
A major one.
Last Sunday, when I landed in Palm Springs, I overheard a few people talking to another passenger about how they were EMR / EHR consultants for a major software vendor who traveled back and forth to a local hospital every week. I didn't ask which one.
Anyhoo, back to the story.
I booked an appointment with the clinic for 3:15. I arrived early as they suggested. I hadn't used a pharmacy clinic before. There were two check-in kiosks. One of the two was stuck on some sort of failed Windows reboot black screen of BIOS errors and “press esc. to continue” errors.
The second touchscreen kiosk was working, so it allowed me to check in. I'm glad they had hand sanitizer right there, given that kiosks anywhere are germ-ridden. That's a special confirm when sickness is more prevalent.
The nurse practitioner (NP) pleasantly called me back at about 3:18, a few minutes after the previous patient stepped out. Not bad. I appreciated the promptness. She was probably cleaning and prepping for me, I figured.
I chuckled, thinking about a scene from a recent episode of the show “Silicon Valley,” where Richard has an idea while at the doctor, so he starts writing it on the exam table's paper covering that he's sitting on.
The doctor expresses his displeasure about writing on the paper.
“You change this after every patient, right?” Richard asks.
“I guess I'm gonna have to now,” he moans in response.
I described my symptoms to the NP and she paused, I guess realizing I'm not dying, to collect my insurance information and identification. She turned her back to me to type into the electronic health record (EHR). Which EMR? A major one (I could see the logo on screen over her shoulder).
When I've seen hospitals do “Lean Design” with exam rooms or patient rooms, the best practice is to have things situated so the doc or NP can type and face the patient. Not here at WalVS.
She started to say, “Oh there's a bug….” and I finished the sentence in my head. I was surprised when she finished it with, “… a bug on the wall,” so I told her, “I thought you were going to say a bug in the software.” I was just making a joke, not looking for blog fodder.
She laughed and started explaining some of her frustration (which was fine since I wasn't dying), while she typed away into the computer and scanned my ID cards. Remember, she was the only employee in this “box,” so she had to do it all herself.
The NP explained how the EHR worked OK, but it seemed to be designed for an inpatient setting.
She complained (rightfully so) that they hadn't really given any training in how to use the system. She said her first patient visit with the new EHR took an hour between her figuring out how to use it and there were some technical problems where the scanner wasn't properly sending information into the cloud-based EHR.
I hear of this happening a lot in healthcare. Health systems spend tons of money (sometimes hundreds of millions of dollars) on EHR systems, but they skimp on the training. That's one of those situations where the “cost / benefit” analysis seems faulty. In the short-term, the health system knows much they are “saving” by skimping on training hours and effort. That's short-term and known. What's longer-term and unknown is the cost of not doing enough training.
What's the cost of not properly aligning workflows and the EHR? What's the cost of not getting input from those who are going to have to use the system on a daily basis?
I doubt the NP is complaining about this to every patient. I happened to express some interest and I told her that I was a consultant to hospitals.
She explained some further anxiety and the dysfunctions (my term, not hers) that cause it.
“They're cutting our appointment times even shorter…”
She was being resilient and laughing… not because it's funny…
“You have to laugh sometimes or you'll go crazy.”
I half-jokingly offered to bill her for a counseling session and she laughed.
It seems like this major corporation is making decisions from a distance that affect their front-line caregivers. Are the leaders “going to the gemba” to see some of these problems first hand? To get feedback?
Is it fair to give them EHR tools that slow down their work (as the NP said) while also asking them to see more patients per hour? That's a dumb question of me to ask. Of course it's not fair.
I told the NP that I hear complaints about EHR systems everywhere I go, regardless of the vendor. It's not as simple as blaming the problems on the EHR software vendor… these are systemic problems involving the collaboration (or lack thereof) between health systems, software providers, and consultants.
During a recent visit to my regular primary care provider, I saw the Medical Assistant (MA) write my weight down on a sticky note. She then carried that into the exam room to enter it. Ah, the “electronic” medical record at its finest.
Back to my “NP in a box” visit… the phone rang and, again, given that I wasn't a life-or-death case, she answered it and had a quick medical discussion with somebody.
She apologized and said,
“Because we all work alone, we sometimes have to call each other to get input.”
The NP added that she has to do everything herself, including cleaning the rooms. She said:
“I'm not above doing that sort of thing.”
She also mentioned that nurses at her previous hospital employer had to do tasks like that. I explained that, from my hospital work and observation, there's a time and place for being a good team member, but we generally want nurses to spend most of their time being nurses. We shouldn't cut housekeeping staff so low that nurses are being distracted from bedside patient care.
“Well, they fired all of the medical assistants here.”
That's probably another corporate decision that was made without getting input or seeing the impact of such a change. It's easy to ask the NPs to do more in less time… harder to actually pull that off.
So, I went on my way with a prescription and a few over-the-counter recommendations. I asked the NP if I needed to jot those names down (which type of Mucinex?) or if it would be in some visit notes. She said that I didn't have to write it down… “We don't make you do homework.”
As I waited for the pharmacy side of the house to fill the prescription, I started to shop for the OTC medications, I looked at the print out. There were no notes about exactly which recommendations she made. She either forgot to put that in the notes (which is possible, since I was distracting her with our discussion) or those fields aren't printing properly. I don't know.
Do you run across similar situations in your healthcare workplace or during your experiences as a patient? What can we do about this?
I'm looking forward to reading some advance material for a book that I've been asked to write a foreword for over the coming months:
Lean Health IT: A Practical Guide to Deploying and Optimizing EHRs Using Lean
The book is due out in February 2018, if there are no delays.
The other day, I heard about a friend's Lean / Toyota book's publication being delayed. Why? It was blamed on layoffs at the publisher.
Which one?
A major one.
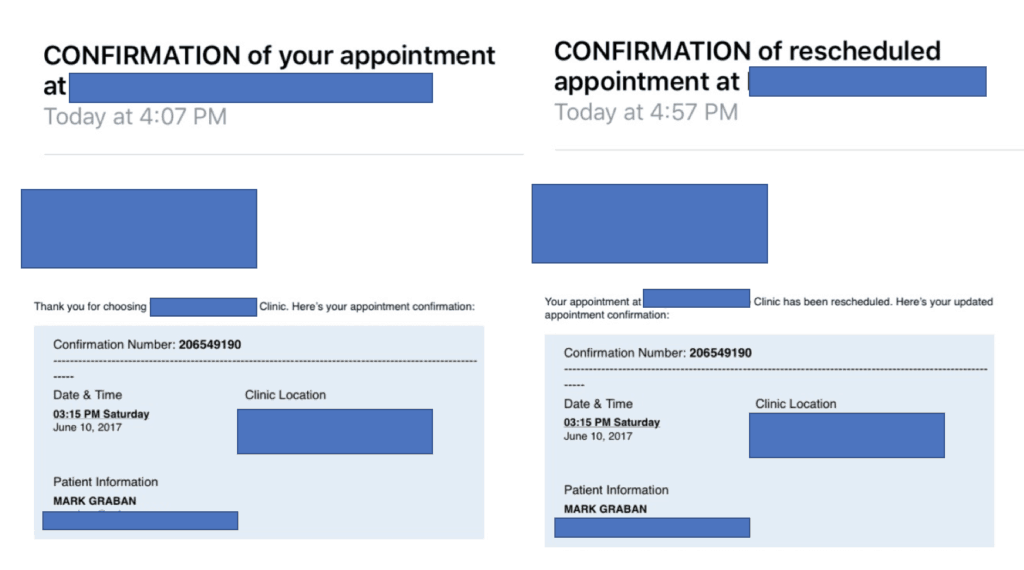
P.S. As a sign of some computer system problems, I received two emails SUNDAY afternoon from the company. I wondered why I hadn't received an immediate email confirmation of my appointment request. The confirmation arrived at 4:07 PM Sunday, about 28 hours after I booked this and over 24 hours after the actual appointment. At 4:57 PM, I received a “confirmation” of an appointment reschedule that didn't happen… because I didn't request it.
Oh, and get this… the NP says they are going to shorten and squeeze her appointment times. But, they might also punish the providers if they get poor marks from patients about spending enough time with them… as their survey asked:
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s build a culture of continuous improvement and psychological safety—together. If you're a leader aiming for lasting change (not just more projects), I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s talk.