Last month, I saw this article from the publication Hospitals & Health Networks (H&HN), where they summarized a speech given by the legendary Dr. Don Berwick at the National Patient Safety Foundation annual conference:
Don Berwick's 7 Roadblocks to Improving Patient Safety
Berwick is, of course, the founder of the Institute for Healthcare Improvement (IHI) and he was also Administrator for the Centers for Medicare and Medicaid Services (CMS) under President Obama.
The IHI and NPSF recently announced a merger back in March, actually:
But back to Berwick's seven points (and see his detailed remarks via H&HN).
1) Displacement by other concerns
I've seen too many surveys where C-level healthcare executives are asked what their “top concerns” are and patient safety is never at the top of their list.
Yesterday, I tweeted about another survey (from the Advisory Board) that doesn't even surface patient safety as a top concern:
It's a shame #patientsafety wasn't on this list — What 183 C-suite executives told us about their top concerns https://t.co/VBOfxAvJn9
— Mark Graban (@MarkGraban) June 26, 2017
I agree with Berwick that the connections between staff engagement, patient safety, and cost should be clear…
2) Illusion of completeness:
It's easy for executives to say, “We've already done patient safety,” as they might also (incorrectly) say, “We implemented Lean last year.”
As Berwick said:
The concept of safety as a box-checking enterprise, where we start and finish, is lethal to patients of the future.”
3) Incentive theory:
Berwick's roots in working directly with Dr. W. Edwards Deming show here. Healthcare professionals have strong intrinsic motivation to not harm patients. As Deming, Alfie Kohn, Dan Pink, and others would point out, more incentives or better-designed incentives aren't the solution we need.
4) Metrics glut:
I agree that most organizations' executives have too many metrics — not just around patient safety and not just in healthcare). Remember, KPI stands for KEY Performance Indicators.
As I've blogged about, the Lean process of “Strategy Deployment” helps leaders prioritize key measures of an organization's health and progress.
5) Separation of safety from quality:
Berwick says:
“When people say ‘quality and safety,' what I hear is ‘fruit and bananas.'
Berwick says safety is a subset of quality. I don't hear most organizations talk that way, so I'm one of those people who says “safety and quality.”
I get his point that patient safety is one form of quality (just as patient satisfaction and service is another dimension of quality).
Too many executives think they have delegated quality, just as they've delegated safety. As Deming said, “Quality starts in the boardroom” (and safety too… even if that's redundant per Berwick).
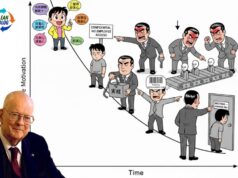
6) System literacy:
Berwick says we need to become better systems thinkers. Lean is one way to break down silos, as Dr. Deming taught.
7) Academic attacks:
Maybe Berwick means articles like this:
where academics are “positioning themselves as critics of the good-hearted work going on…”
H&HN quotes Berwick as saying:
“We have to remove the chaos,” said Berwick, who also served as administrator for the Centers for Medicare & Medicaid Services. “We know how to do it, we've made progress. In the next 20 years, I don't think we should be able to say we've learned what we need to know, I think we need to say, now what do we need to do?”
There's been progress… in pockets throughout healthcare (as I've collected some stats and stories here). We need more progress, more widely. Nobody's perfect, but some organizations have made great strides, while others lag behind.
When I asked Paul O'Neill once what held back patient safety progress in healthcare, he said, without missing a beat: “Lack of leadership.”
Hear my podcast with him, where he said:
“I honestly think the skill shortage in our society, maybe in the world of civilized people, is real leadership.”
What was O'Neill's prescription for improvement?
“I would urge Boards of Directors of health and medical care institutions, hospitals, and nursing homes to ensure the day-to-day operational leader is supportive of the idea of establishing theoretical limit goals for everything that goes on in their institutions. Because I think if Boards of Directors urge the people who are day-to-day responsible for care delivery, it might provide some stiffening of the backbone of those who are supposed to lead institutions to habitual excellence.”
Facebook reminded me, also, that it was a year ago yesterday that I blogged about the Emily Jerry story as told by her father Chris on Fox News:
Sorta Live Blogging Fox News “Beware! Danger at the Doctor” (Part 1)
What do you think is holding back patient safety progress?
If you’re working to build a culture where people feel safe to speak up, solve problems, and improve every day, I’d be glad to help. Let’s talk about how to strengthen Psychological Safety and Continuous Improvement in your organization.