I'm always happy to see success stories where healthcare organizations solve problems that matter through Lean concepts, practices, and principles. Today, I'm blogging about two articles I saw about this recently.
One of the problems that needs to be solved in healthcare is long waiting times, whether that means waiting for care in the emergency department, waiting for an appointment, or waiting for test results.
The first article I saw is from Ireland:
At last, one hospital has slashed its waiting lists
With a sub-headline of “Beaumont patients offered prompt surgery in Cavan, thanks to Toyota.”
From the article:
“A new management system for dealing with waiting lists in Cavan Hospital – based on an efficiency model pioneered by car giant Toyota – has been so effective that patients on Beaumont Hospital's lengthy waiting list are now being offered the choice of having their surgery done immediately in the north-east.”
Again, it's great to see waiting times reduced or eliminated. As the article says,
“While the average length of a hospital stay in Ireland was 6.1 days in 2014, in Cavan it was 3.87.”
It's great to reduce length of stay and I'll assume the hospital is doing it “the right way” and isn't pushing patients out the door too soon. A shorter LOS means better throughput for patients (which also affects the operating rooms)… more throughput means shorter waiting times.
I want to highlight how it's wrong to just refer to Lean or the Toyota Production System as “an efficiency model.”
Look at Toyota's own corporate web page on TPS.
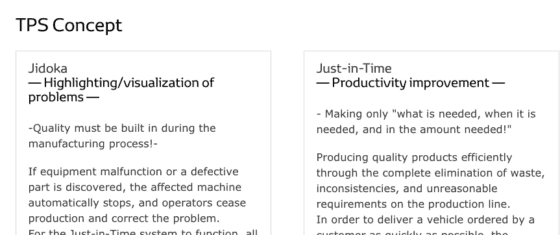
The two pillars are:
- Jidoka — building in quality at the source
- Just-In-Time — improving flow
Hospitals (or their consultants) often get it wrong when they think or say that Lean is just about cost.
Lean and TPS are about quality AND flow. You can't have one without the other.
Improving flow (the right care at the right place at the right time) isn't about “efficiency” (as measured by outputs divided by inputs). A focus on that traditional measure of efficiency often leads to an organization wanting to keep everybody busy (or every machine busy)… which is really bad for flow.
The Lean focus is on FLOW — not having the patient be idle is the main goal. Sometimes that requires staff or equipment actually be idle… 100% utilization leads to very long waiting times, as basic Industrial Engineering and queuing theory would teach us.
Hear Mark read this post — subscribe to Lean Blog Audio
Productivity, the word Toyota uses, can be an end result.
As Toyota explains:
“Based on the basic philosophies of jidoka and Just-in-Time, the TPS can efficiently and quickly produce vehicles of sound quality, one at a time, that fully satisfy customer requirements.”
The article from Ireland, frankly, gets it wrong:
“Lean is a management model first used by Toyota in the 1950s and created to cut costs and improve efficiency by eliminating waste.”
Where is the mention of quality there? Note that the Toyota webpage does NOT contain the word “cost.”
The Irish article also says:
“Canada and Australia are two countries that have used the system to virtually eliminate waiting lists.”
At least for Ontario, a province in Canada, that statement is completely incorrect, as you can look at the government's own data on patient waiting times.
Speaking of Ontario, here's the second article:
Doctors go ‘Lean' to cut wait times, improve health-care efficiency
Here we go, just efficiency? Improving quality is a great way to improve efficiency and reduce waiting times. Does the article mention this?
“Family doctors in Eastern Ontario are learning the business lessons of banks and carmakers as a way to make their practices more efficient.”
That's sort of weird to mention banks before automakers, but it does help make the point that Lean is not just about improving the way we build cars.
“Nearly 30,000 patients in Eastern Ontario will see the benefits of things like “queue theory” and Toyota's “Lean manufacturing” philosophy thanks to a three-year project aimed at cutting wait times and improving the efficiency of front-line health-care providers. The training is being provided for free by the Champlain Local Health Integration Network and the philosophy behind the project is simple: Helping people stay healthy longer is one of the best ways of reducing the burden on the health-care system down the road.”
How does the article define Lean and TPS?
The “Lean management” system pioneered by Toyota improves efficiency by eliminating unnecessary or duplicated work. The solution can be as simple as putting a printer in each examination room, saving the doctor a minute or two spent at each appointment walking to a central printer. Those minutes add up over the course of a day, Jackson said.
Sigh. No mention of quality, unless they are including that as a form of “waste” or as a type of “unnecessary work.”
I do like how they seem to be engaging staff in improvement:
“A lot of [staff] feel they're drowning in work. That's where we can provide support. We can pull them out of their practice for an hour or two and take a look at the forest, not just the trees, and think about ‘what might make your work easier?'”
That's a classic Kaizen starting point question. How can we work together to make your work easier? Solving those problems usually leads to improvements in both quality AND flow.
As one doctor said:
“While some of his colleagues have wait times for appointments of four weeks or more, Sardana tweaked his practice to meet his goal of having wait times of less than five days. Though his consultations with Jackson are done, the tools he learned help him keep his practice running smoothly.”
I applaud their efforts to get waiting times down… again, that's a great example of solving a problem that matters. Now, will they also work on safety and quality?
The Ontario program is called “Primary Care Quality Practice Facilitation,” so let's hope there's some quality improvement.
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s work together to build a culture of continuous improvement and psychological safety. If you're a leader looking to create lasting change—not just projects—I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s start a conversation.







![When Was the Last Time a Leader Around You Admitted They Were Wrong? [Poll]](https://www.leanblog.org/wp-content/uploads/2025/07/Lean-Blog-Post-Cover-Image-2025-07-01T212509.843-100x75.jpg)
Dear Mark,
Your article really shook me up to re-think what am I doing? We have been doing the similar things of cutting down wastes, eliminating costs etc. And then I happen to read this article.
So, how would you define quality? Clearly, in healthcare, the customer doesn’t receive any tangibles, or rather not much of the end product is tangible. Only tangibles that the patient has are waiting times, LOS, Early mobilization etc. So, going by the voice of the customer, those are the areas where we can apply Lean principles, and improve quality (as a function of customer’s perception).
Also, the surgery outcomes majorly depends on the surgeons handiwork, although there are systems around it where we can standardize and improve the outcomes, but the major part of it still remains an art.
Shall be great to hear from you.
Puneet Mehta
Thanks for your comment, Dr. Mehta. I guess I’d ask how you define quality? How do your patients define quality?
We can think of service quality, often measured in terms of patient satisfaction. Systems and processes contribute to this. Waiting times are a factor in this. Staff attitudes and their tone or the way they interact with patients matters too. A lack of efficiency (too much waste, too much effort in their work) can lead to staff being stressed, which can hurt service quality in different ways.
Flow and quality often go hand in hand. Our goals and measures are often interconnected.
Think also about clinical quality. Many results and key measures are the result of systems and processes, not just the skill of the surgeon, doctor, or nurse.
As I shared in the 3rd edition of “Lean Hospitals,” some measures of quality impacted by Lean include:
Medication errors would be a measure of quality, as would be the quality and temperature of the food served to patients. Many of these quality problems can be addressed through Lean methods, problem solving, and management practices.
I hope that helps.
Hi,
My question is about value in healthcare. The first principle in lean thinking is to specify value. How exactly is value identified and measured in healthcare? Is there an objective method to measure value in a health care setting?
Value is probably more of a conceptual thing. If value = health and quality of life, I’m not sure how you precisely quantify that.
You can probably measure contributors to value… such as time a nurse spends working with patients (generally adding value depending on the detail of what’s happening) vs. activities that are clearly NON value adding (or waste), such as searching for missing supplies and equipment, rework, etc.
Why do you ask that question? I’m curious as that might help with our discussion.
Thanks for your reply. I am a PhD student looking at patient flow in emergency departments using process mapping. The question of value in healthcare came up as a result of reading on lean thinking and value stream mapping. The VSM identifies value adding and non value adding steps. The non value adding steps seem to be easier to define and measure (eg waiting times) than value adding steps. From an economic view, value in health refers to the health outcomes achieved relative to the cost of care. But I’m not sure if this is what is meant by value in lean thinking/VSM.
It’s easier to measure how long a Value-Added step takes. That doesn’t always equate to Value as defined by the customer.
I’d agree that Value means health outcomes, quality of life, etc. That’s harder to measure. The “cost of care” for a particular episode of care or a particular patient is often hard to measure too (considering how to allocate overhead, etc. for a true cost).
It’s easier to improve flow by reducing time delays… or even to measure quality in different ways than it is to directly measure “value.” Value is more of a concept than a measure.