Mark's Note: Today's guest post comes via my friends at the ThedaCare Center for Healthcare Value, who suggested this case study from Salem Health. You might remember my post from 2012 where I shared a video of some of their senior leaders talking about going to Japan. At the bottom of this post is an 18-minute long video that was shared by the Center.
By Debbie Goodwin, Salem Health
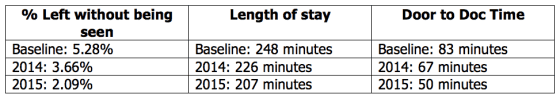
Decreased patient experience scores, increased ED length of stay, increased left without being seen rate and increased time from the patient presenting to the ED until time to see a doctor were all problems that the Salem Hospital Emergency Department was experiencing in 2014.
Along with these problems, the ED continued to see an increased census along with an increase in the number of emergent cases. Over the past ten years, the number of inpatients who are admitted through the ED has grown from 22% to 66%.
Due to these problems, improving ED throughput was selected as one patient experience strategy in fiscal year 2015. The challenges faced in our ED presented us with an opportunity to use Lean concepts and tools to improve our processes and outcomes.
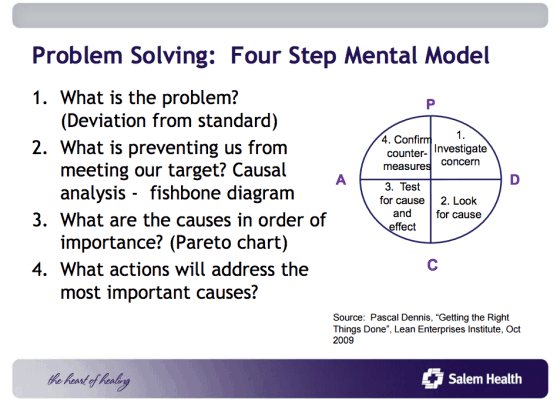
Dr. Paul Gramenz, Medical Director of the Salem Emergency Physician Service, was a key stakeholder and participant in the ED throughput improvement work along with the ED leadership. Various other stakeholders were instrumental to helping problem solve the throughput challenges. Leaders and staff from a variety of areas such as Imaging, Lab, Patient Transport and Access Services joined together to view the work from the patient perspective. Using “Four-Step Problem Solving,” based on the scientific method of Plan-Do-Check-Adjust, teams ran multiple tests of change over the course of the year.
One significant test of change was implementing “Provider at Triage.” Dr. Gramenz says, “Of all the tests of change, Provider at Triage had the greatest impact.” The Provider at Triage moves the provider and patient interaction to an earlier point in the process, helping to expedite care of the patient.
Provider at Triage is open 10 a.m. to 10 p.m. each day and is staffed with two physicians, each working a six-hour shift along with ED nurses and technicians. Nurses screen the patients in triage and based on standard criteria to determine the less emergent patients who can be seen by the provider in the triage area. With this work done up front, the less emergent patient does not have to go to the back of the ED and occupy a bed that is needed for a more acute patient.
Heather Cofer, RN and ED Nurse Manager, said there were several key things that were important to the success of some of the tests of change. “Solidifying the triage process was an important foundation before testing Provider at Triage. Also, we couldn't keep up with the volumes from 10 a.m. to 10 p.m., so we realized we needed another process to screen patients privately. There was some math involved to determine why we chose the number of rooms, staff, and providers needed.”
Implementation of a “results pending” area in the lobby has also freed up rooms in the back of the ED for more acute patients, creating better flow within the department.
Another example of a test of change was the Patient Transport Department starting a “bus route,” which was a new way for them to do their work. Rather than waiting for a call to get a patient for Imaging, the Patient Transport Department actively rotates through the ED to take patients to and from Imaging. Dr. Gramenz along with others realized “there was not a standard process for patients to transport to and from Imaging and implementing the bus route led to better patient flow.”
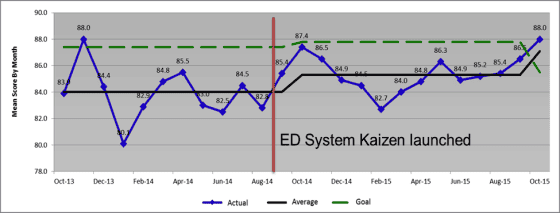
Excellent results were obtained from the work done in 2014 and continued efforts extend into 2016:
Patient Experience
- 2013: mean score: 84.0, 71th percentile
- 2014: mean score: 85.3, 68 th percentile
- 2015: mean score: 87.1, 92th percentile
Impact
Having the foundation of Lean fundamentals in the organization supported this “system kaizen” work. Standard Work is an important component of the overall ED patient flow.
Now, as volumes in the ED continue to rise, the processes are well defined and executed. The “left without being seen” rate may go up slightly on a high volume day, however the rates are not near as high as any of the rates seen before doing the system kaizen.
The Lean concept of Visual Management contributes to people knowing, on a real time basis, the current status of ED throughput, which enables better decision making in the moment.
There are still improvements that we can make to patient flow and next steps may include the connection between the ED and inpatient admission.
Coming to agreement on the key measures for the ED throughput system kaizen took some time. However, once the measures were identified, it's been “easy” to see the impact of the work. It was important to take the time to clearly define the problems in the ED with data. Initially, the physicians were skeptical to make changes, however Dr. Gramenz noted, “Once they saw the data, it didn't lie and it was clear we needed to improve our patient flow. The data also show we are being successful.”
About the Author
This article was submitted by Debbie Goodwin, RN, BS, MSN, a Kaizen Learning and Development Consultant at Salem Health in Salem, Oregon. Salem Health holds memberships with both the Healthcare Value Network and the Clinical Business Intelligence Network that are managed by the ThedaCare Center for Healthcare Value. These Networks unite healthcare leaders who share a commitment to providing high-quality, cost-effective care through the application of lean concepts. To learn more visit createvalue.org.
Video:
(now “private”)
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
If you’re working to build a culture where people feel safe to speak up, solve problems, and improve every day, I’d be glad to help. Let’s talk about how to strengthen Psychological Safety and Continuous Improvement in your organization.