Yesterday, I wrote Part 1 of this post on the Cleveland Clinic Improvement Model.
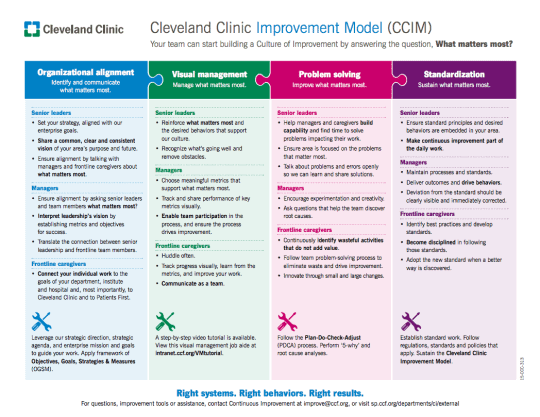
Part 1 covered the left hand half of the model, with Organizational Alignment and Visual Management being the key themes.
Once you have alignment, measures, and visual management in place (with big doses of communication, leadership, and teamwork), you're better situated to solve problems.
When you're working on improvement things that matter, it's easier to engage people in that process. That's one reason I like rallying people around a topic like safety or a broader notion of improvement instead of saying “let's go implement Lean.”
Problem Solving
As I'm going to write about in a future post about my site visit, I saw A LOT of problem solving and improvement… accomplished by engaging the people who the work, coaching and supporting them.
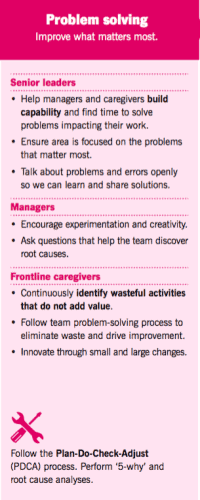 The problem solving portion of their puzzle is built on a foundation of the PDCA model – Plan Do Check Act (or it could be Plan Do Study Adjust, or PDSA). I think they're hinting at an idea I've written about, that “the 5 whys” is not the only step in root cause problem solving (and it's not always magically the number 5).
The problem solving portion of their puzzle is built on a foundation of the PDCA model – Plan Do Check Act (or it could be Plan Do Study Adjust, or PDSA). I think they're hinting at an idea I've written about, that “the 5 whys” is not the only step in root cause problem solving (and it's not always magically the number 5).
I like how Cleveland Clinic, like Toyota, emphasizes the need to “build capability” and develop people. It's not just about solving problems today, but also building capabilities that allow people to be better at solving problems in the future. That's one reason why effective leaders in a culture of continuous improvement avoid giving answers to their employees… as that might help in the short term, but it also stunts the growth of others (and can demoralize people who want to think for themselves).
It's also critically important that executives set a tone that makes it OK to managers to free up time for people to work on improvement. “We don't have time for improvement” should be a problem to solve, not an excuse to hide behind, as I talk about in this video.
Again, there's a focus on “what matters most.” It would be great to see that in action consistently, rather than people just reacting to whatever fires pop up around them. Maybe I'm mixing the metaphor with “whack a mole management,” but you know what I mean.
Executives also have to create an environment where people can talk freely about problems, mistakes, errors, near misses, and the like. “No problems is a problem,” as Toyota says. “Having no problems is the biggest problem of all,” said Taiichi Ohno.
Leaders need to encourage experimentation (in a structured PDSA way… or an 8-step problem solving model), which means sometimes we'll “fail” or things won't work out as expected. Those are learning opportunities… but that's not an excuse to be wildly irresponsible with Kaizen, either.
Frontline staff play a very important role in problem solving, but they need to be coached by managers and, sometimes, by Lean specialists. I'll write about that in my blog post(s) about my visit to Cleveland Clinic, as that active and intentional coaching is a big part of their model.
Standardization
The last piece of their puzzle is “standardization.” I'll note that it's not listed first. Standardized work is a means to an end; it's not a primary goal to standardize for the sake of standardizing.
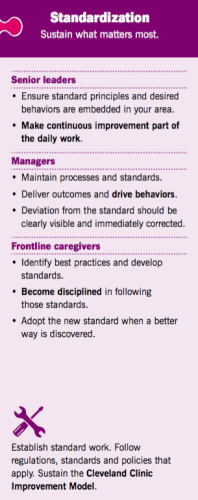 The first bullet point for “senior leaders” is a bit unclear to me. I hope it means “lead by example” in the spirit of standardized work applying to everybody in the organization in different ways (as we see at systems like ThedaCare and Baylor Scott & White).
The first bullet point for “senior leaders” is a bit unclear to me. I hope it means “lead by example” in the spirit of standardized work applying to everybody in the organization in different ways (as we see at systems like ThedaCare and Baylor Scott & White).
I love that they've emphasized the role of continuous improvement here, in that standardized work is never meant to be static or permanent.
But, at the manager level, this also needs to be the focus — not just maintaining standards, but also helping improve those standards and methods. “Deviation from the standard” being “clearly visible” is the Visual Management method, as discussed yesterday. Charts and metrics don't make deviations immediately visible, but good Visual Management does.
I like how managers are not just expected to deliver outcomes and results, but also to focus on the right behaviors (and I'd add processes) that drive results. Lean is not a matter of “get results, no matter what.” It's more about “the right process drives the right results.”
For staff, they need to follow standardized work in a “disciplined” way, but also participate in the development of new and improved standards.
The Whole Puzzle
Again, the image from Cleveland Clinic is not just four pieces… it seems like a system. It all fits together and it seems like it would be mutually supportive.
If you're trying to learn from the Cleveland Clinic model, I'd suggest:
- Adopt the ENTIRE model
- ADAPT this model as it makes sense for your circumstances
- IMPROVE the model over time
- or, CREATE your own based on the process they used
What do you think?
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s build a culture of continuous improvement and psychological safety—together. If you're a leader aiming for lasting change (not just more projects), I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s talk.
Join me for a Lean Healthcare Accelerator Trip to Japan! Learn More










[…] In part two of this post, we’ll discuss Problem Solving and Standardization in more detail. […]
Nice model. Under problem solving it shows a Senior Leader responsibility to facilitate problem solving. Sadly many senior leaders in healthcare are not adept problem solvers so I am wondering about the work needed to enable senior leaders.
Also, just a couple of years ago Cleveland Clinic was touting their continuous improvement program under Darryl Greene that was much focused on projects and ROI and now I see Mr. Greene is no longer with the organization. This new model seems a departure from the previous efforts so I am wondering what the linkage is and if this is an evolution of those prior efforts, something much different, or a parallel initiative.
Mark its an honor to have you discuss the CI / performance management model at the Cleveland Clinic. I am fortunate to be one of the administrators that started with Darryl Greene and Nate Hurle back in 2005. My institute was one of the first to work with the frontline teams using “Fastrac” and visual management tools brought to the Clinic by Darryl Greene. The CI model introduced back then is the model foundation for the work we do today. To answer blogger B.S. I would say the model in this article is an evolution of our work from that time. Today the Cancer Institute is one of the few that have the “culture of improvement ” starting at the frontline ->middle manager-> top administrators. Chad Cummings and Kelvin Vilamil, CI director and CI specialist, helped us create the true organizational alignment that drives the model today. B.S. you are correct leadership training is still and I think will always be ongoing. We have succeeded in developing the “CI culture” but there is more , its the continuous work of developing leaders to improve sustainability. I would like to thank Darryl for bringing the tools to me and my team, but a huge thank you to Chad and Kelvin for helping us evolve our organization throughout our journey. Our focus is always on the patient and these tools and concepts help us achieve out value based care goals. Mark if you are ever in Cleveland again I would love to show you the rest of the work at the clinic.
Thanks, Kim, for your comment. I would love to take you up on that offer sometime.
Interesting model and great information. I did not find the results/outcomes of this model showing significant changes of the KPMs or other indicators. Could you please let me know how can I find them?
Hi Sima – Thanks for your post. Our use of the model has grown since this blog was posted, and we now have around 10,000 caregivers applying the model. Examples of results can be found in many places. Here are a few examples: https://createvalue.org/no-more-projects/
https://www.youtube.com/playlist?list=PLMG0zKOgNqNnnoEXIodo7vO6GRiwm4oL8
Comments are closed.