Back in November, I had a chance to meet Nate Hurle, from Cleveland Clinic, as he was giving a presentation about their work with Lean and continuous improvement. As we chatted, I mentioned that I'd be in Ohio in early December, as I was going to visit my grandfather who lives in northeastern Ohio (he's almost 93!). Nate was kind enough to invite me to spend a day with him and two sites within Cleveland Clinic.
I'm working on a blog post about my visit there, but since that post is going to be pretty long, I'm going to share first some thoughts on their improvement models and frameworks.
The system has a model called the “culture of improvement.” You can read about this via a post on the LEI website. It's not only about the “tools of improvement,” but the culture and leadership that's required for improvement to happen… to build and sustain a culture of continuous improvement.
They also have something called the “Cleveland Clinic Improvement Model” or CCIM. See a PDF or click on the image below for that larger PDF view.
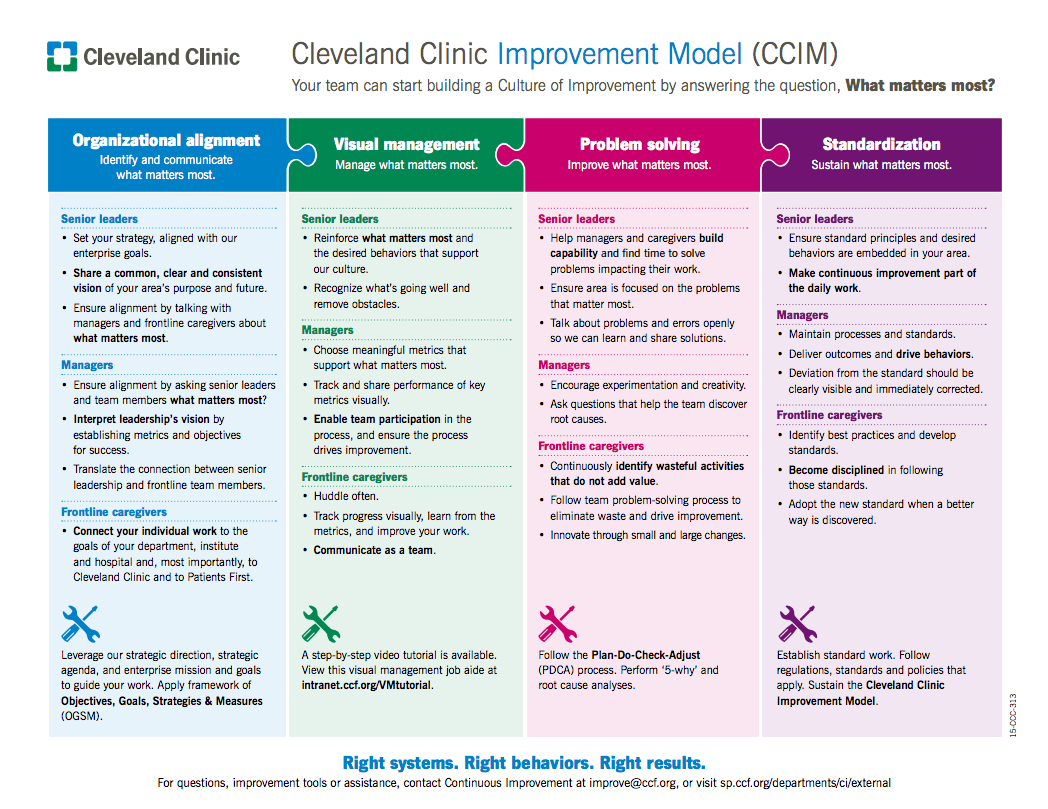
It's a dense model, but there's a lot to like.
First, up top, look at the branding. It's THEIRS… it's the Cleveland Clinic model. There's something to be said about staking a claim of ownership. Out there, you see some organizations call what they're doing “Lean” or “Operational Excellence,” or the like. But you also see names like “ThedaCare Improvement System,” “Michigan Quality System,” and the “Virginia Mason Production System” (although I think it's not helpful to use the word “production” in healthcare). People like to be a part of something that's theirs… they can create it.
Other organizations don't have to copy it exactly. We can learn from others, but adopt and adapt to our organization. It probably wouldn't be helpful if an organization went to visit ThedaCare and came back to do “the ThedaCare Production System” at MidWestRandom Health System. ThedaCare people say you can learn from, but don't copy.
Calling it an “improvement” model is key. It's easier to rally people around improvement or quality than it is “performance excellence” or something more jargony.
And, it's a “model.” As George Box famously said,
“All models are wrong but some are useful.”
Cleveland Clinic starts by asking “what matters most?” That's a great question. It's a variation of the John Shook / LEI question of “what problem are we trying to solve?” I've heard Toyota people talk about the questions we NEED to solve. What's critically important? Patient safety. Quality. What's strategic? Strategy deployment can help frame the need for improvement and our goals.
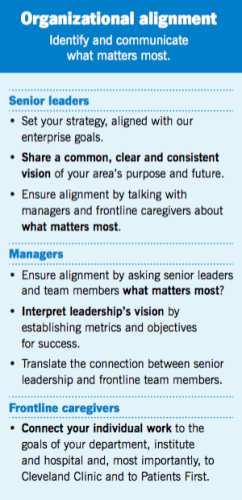
Organizational Alignment
Strategy deployment isn't about forcing goals on people… it's about creating alignment. Alignment between goals and actions, alignment from top to bottom, and alignment across the organization.
Cleveland Clinic starts there, with the step of “identify and communicate what matters most.” Even if executives have a brilliant strategy, it will most likely fail if the organization doesn't understand said strategy and the need for change.
Cleveland Clinic shares tips for executives, managers, and staff in the blue part of the diagram.
I'd suggest the burden is primarily on senior leaders. They need to initiate discussions with middle managers and ENCOURAGE them to push back or disagree rather than just accepting top down communication of strategy. Asking questions and having open, honest discussion is important with Lean.
Frontline caregivers can't connect their individual work to the broader organization if their leaders (at all levels) aren't communicating with them in a bi-directional way. Frontline staff have to be encouraged and empowered to work cross functionally instead of being pressured to suboptimize their silo.
It takes real leadership commitment for a phrase like “Patients First” to be a daily reality and not just a slogan.
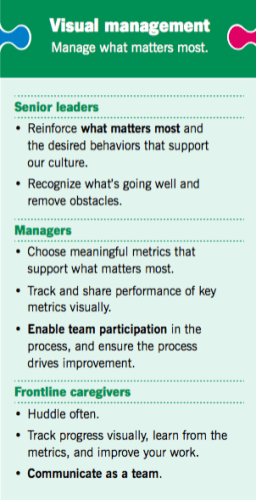
Visual Management
The second piece of the CCIM puzzle is “visual management,” a topic I love to write about.
Leaders are encouraged to “manage what matters most.” It's a really popular expression to say “what gets measured, gets managed.” I like the notion of “what matters gets managed.” It's probably more like “what matters gets measured, so it gets managed.” But. W. Edwards Deming always reminded us that some of the most important things are immeasurable.
Cleveland Clinic emphasizes measurement and the visual management of said measures… but I'd point out we have to be careful to not misinterpret measures or make bad decisions based on them. And, I'd add that there's more to visual management than charts and metrics.
The finer points of the Cleveland Clinic model are great:
- Recognize what's going well and remove obstacles
- Enable team participation…
- Huddle often
- Communicate as a team
Throwing metrics up on the wall can be dysfunctional if you're not doing those things.
In part two of this post, we'll discuss Problem Solving and Standardization in more detail.
What do you think of this model? Does your organization have something like it? Something better?
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation:










Doing the work to develop the model will have had a value in itself, assuming that it was a participatory process. I like the local identity to the Cleveland Clinic work.
It’s true, of course, that metrics are only one kind of visual management, and then only if they are used to manage and improve. David Mann commented that ‘visual controls amount only to wallpaper without the discipline to insist they are taken seriously and used as a basis for action’. From the problem solving and standardization sections in the Cleveland model, it certainly sounds as if they are trying to do that.
A significant value for us in using this model is that we “demystified” what Continuous Improvement is for our caregivers. It was a significant undertaking by our entire CI team and created significant ownership of the model.
Appreciate Cameron’s note. Yes, the process was extremely valuable for our own development as a team and as an organization We did an A3 on the problem (you can read more in the LEI article). From the A3 we started testing countermeasures, and literally hundreds of Cleveland Clinic caregivers contributed to the model through their hard work, best thinking, and candid feedback. The model is our countermeasure, developed through our own assessment of current state, root cause analysis, and lots and lots of PDCA. It is very “us” – and I think that is why it resonates at Cleveland Clinic.
We do not know if our model will solve someone else’s problem – but if someone wants to try it we would be extremely interested in hearing how it goes!
Thanks for that additional perspective about the process to create the CCIM, Lisa.
It seems similar to value stream mapping… the process to develop the map (engaging people, going to the gemba, getting different perspectives) can be more valuable than the end product. Or, I guess I’d say that some people focus too much on the end product map and short change the process it takes to get there.
It’s quite possible that you sharing this model inspires others to borrow or tweak your model… or maybe it inspires them to use a similar process to create their own? It will be interesting to see.
[…] I wrote Part 1 of this post on the Cleveland Clinic Improvement […]
Mark: thanks for sharing this write-up. I like the CCIM for exactly the reasons you’ve talked about. One key distinction I see again and again is successful adoptions of lean models almost always build it into something that is owned by the entire organization– whereas other organizations try “Lean” and end up with incomplete use, flawed understanding, and underlying resentment from frontline staff and providers who are “leaned” on. Great post, and looking forward to reading the second part!
Practical blog post ! I learned a lot from the facts – Does anyone know where I would be able to obtain a fillable a form version to use ?
What do you mean by a “fillable form” for this?
Hi Julieann – We created the CCIM in an excel document and gave it to our marketing folks for formatting.
We do have “fillable” A3 templates (in Excel and Word format) that we often use – would that be of use to you?