 There are certainly many serious problems in healthcare. Let's look at nursing, in particular. It's a rewarding job, but it's far more frustrating for nurses than it needs to be.
There are certainly many serious problems in healthcare. Let's look at nursing, in particular. It's a rewarding job, but it's far more frustrating for nurses than it needs to be.
Nurses often don't have enough time in the day (or in a given hour) to do all of their work the right way in the time available. I've worked with nurses who listed out all of the tasks they were supposed to do in an hour, from rounding on patients, giving medications, etc. and it added up to 80 minutes worth of work to be done in 60 minutes.
THAT'S IMPOSSIBLE.
Nurses are often forced into a position of choosing what to cut corners on. What tasks do you skip or delay? Nurses, thankfully, use judgment to determine what tasks are “lowest risk,” for the sake of their patients. They're also doing so for the sake of their jobs, since they'll likely get blamed and punished for making an error in a bad system. That's not Lean thinking of course, but it's sadly common.
That's bad for nurses and it's bad for patients. It must be fixed.
We have overburdened nurses (and staff in other areas). We have low patient satisfaction and quality that's lower than it should be. Patients' discharges are being delayed. Too many patients are being harmed and killed due to preventable errors.
Some people say (I think incorrectly) that “Lean is all about waste.”
The Japanese word for waste is “muda.”
I think the bigger problem in healthcare is “muri,” or overburden.
Overburden leads to waste. It leads to stress, harm, and higher costs.
What is the Real Problem?
The problem often gets framed as “we don't have enough nurses.”
That's a solution disguised as a problem statement. The solution to “not enough nurses” is, of course, “add more nurses.”
That's not necessarily affordable. We might not be able to recruit more nurses. And, that's not the only way to solve the real problem.
When you hear people say “we need more nurses” (solution) or “we don't have enough nurses” (fake problem statement), we should define the real problem(s).
A better, and more accurate, problem statement might be:
- Patients aren't getting all of the care they need in a timely manner
- Nurses are overburdened and have too much to do
- Patients are being harmed
- Patients are waiting too long to be discharged
Of course, we would want to get more specific and quantify those problem statements in terms of a “gap” to be closed, but let's skip that for now.
We can rally everybody around improving patient care. An objective problem solver would only care about solving these important problems.
There are certain groups that seem to advocate primarily for their solution (more nurses). Unions, for example, benefit from more nurses because that means more dues for them. Do the nurses' unions care about reducing patient harm? Of course. But, some of them seem too stuck on a single solution (more nurses).
What Can We Do About These Problems?
If we're going to solve one of those problems… and not having enough nurse time is one of the causes (or even a root cause), then there are two main countermeasures we can take:
- Add more nurses
- Reduce waste to free up nurse time
There's a lot of talk and research about patient:nurse ratios. Studies suggest that a lower patient:nurse ratio results in better care (or having fewer nurses per patient results in worse outcomes). That seems intuitive.
But, I'd propose the number that really matters is the amount of nursing time available in an hour or a day. How much time do nurses get at the bedside?
Before Lean, it's very common to see that nurses only get about 30% of their time at the bedside with the patient. Increasing this time at the bedside results in better patient care and higher patient satisfaction (and you can see how that would be more rewarding for the patients).
Look at part of this spreadsheet that I created… if we have 24 patients and 4 nurses, that's a 6:1 ratio.
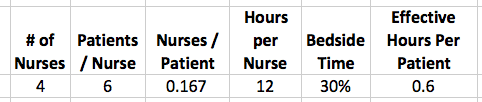
You can do the math of 4 nurses * 12 hours per shift * 30% bedside time / 24 = 0.6 effective bedside hours per patient per shift
Adding Nurses is One Option
If we add nurses, you can see how the hours per patient increases, but you can also see how cost increases (at a burdened rate of $45/hour):
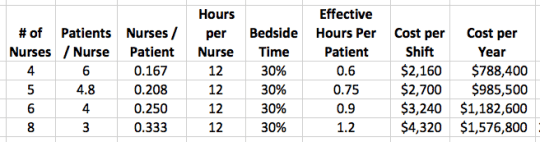
If we double the number of nurses, we get double the time at the bedside (assuming the 30% ratio stays the same). The cost per year has doubled (the cost of that day shift multiplied by 365).
Even if we're “throwing nurses at the problem,” we should look and see if increasing staffing levels by about $800,000 would reduce the cost of poor quality and the cost of longer length of stay.
Throwing people at the problem might not be the BEST strategy, but at least it's a strategy. I'd respect that more than doing nothing and expecting better results.
Reducing Waste through Lean is a Better Option
Lean provides a welcome alternative to just adding nurses. We can reduce waste, which frees up more time for the existing nurses to reapply to patient care.
We can get staff member ideas, through a Kaizen process, to ask them what problems need to be solved to free up their time.
The hospital might run “rapid improvement events” that are focused on making more dramatic changes that would free up time.
We might implement a Kanban system ensures that supplies don't run out. We might install “nurse servers” to make sure those supplies are as close to the bedside as possible.
Team roles and responsibilities might be reconfigured, as we analyze what nurses, CNAs (techs), and housekeeping staff should be doing. Are nurses doing work that should be done by others (and vice versa).
Technology and software might need to be improved. Better communication systems can be put in place. Important information can be made more visual.
There are many, many improvements that can be made that free up nurse time. Virginia Mason Medical Center has increased nursing time at the bedside to 90%.
What happens when we keep staffing levels and the same and increase time at the bedside? The baseline is on the top row:
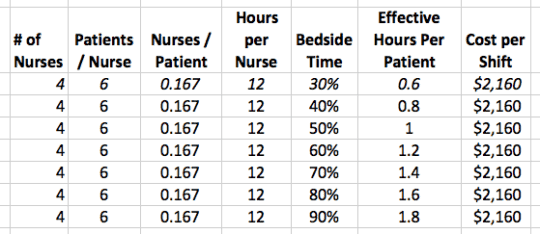
If we can take bedside time from 30% to 60% (in my experience that's very achievable), we can get the same effective hours per patient (1.2) without doubling labor cost.
If we can reach Virginia Mason levels, we TRIPLE nursing time, without adding cost.
Or, if we add one nurse AND increase the percent time at the bedside to 60%, we do even better (1.5 hours per patient).
Here is the spreadsheet I used if you want to download it and play around with numbers yourself (via Dropbox or Google Drive or a Google Doc).
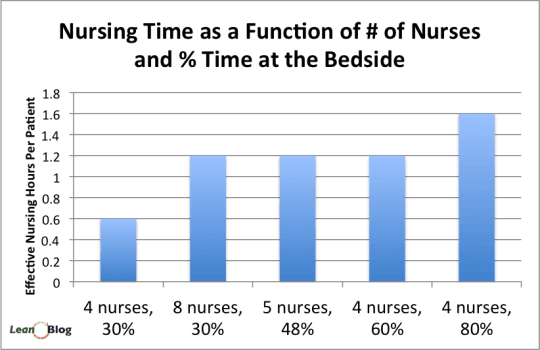
And here is a chart the summarizes the effect of adding more nurses and/or increasing the percentage of time at the bedside.
What are your thoughts on this? What are you doing to free up nursing time using Lean or other methods?
Can we convince people that Lean is not just an alternative to layoffs, but is also an alternative to throwing people at a problem?
Please scroll down (or click) to post a comment. Connect with me on LinkedIn.
Let’s work together to build a culture of continuous improvement and psychological safety. If you're a leader looking to create lasting change—not just projects—I help organizations:
- Engage people at all levels in sustainable improvement
- Shift from fear of mistakes to learning from them
- Apply Lean thinking in practical, people-centered ways
Interested in coaching or a keynote talk? Let’s start a conversation.








![When Was the Last Time a Leader Around You Admitted They Were Wrong? [Poll]](https://www.leanblog.org/wp-content/uploads/2025/07/Lean-Blog-Post-Cover-Image-2025-07-01T212509.843-100x75.jpg)
Interesting article and thanks for bringing up the issue of nursing shortage.
Personally I was directly involved in implementing the lean process and I believe that lean is an effective method to reduce the waste and help improving outcomes.
And if we look closely at the nursing care models ,all of those models provide a frame work to achieve excellence and improve patient outcome.
Nurses had demonstrated agility,flexibility and success when it comes to implementing new models;thanks to the well organized team structures that made this possible.
But sadly every time an organization decides to remove waste the first victim is the nursing devision.
Nurses are compensating for almost every additional expense in healthcare facilities and it is reflected in (Reduced overtime,compensatory time,extra working hours,work overload,compromised patient safety…)
By the next few years and not so long the world will have almost 50% of his nurses retired!!
This means that a massive shortage in nursing is coming soon.
I believe that nurses are not being rewarded as it should be.
I wonder if The international council of nurses had conducted any international survey to asses nurses satisfaction but I can tell the results will be scary!!
I believe that LEAN cannot be tailored and if an organization considers LEAN implementation, it’s should apply it to all it’s sections and divisions ,I believe that they will be shocked by the massive waste that can be eliminated.
I wish after doing so if they would consider rewarding nurses some of that WASTE .
Thank you.
There is a analogous situation in higher ed where the problem (always) is “we don’t have enough faculty.” The solution, of course, is “hire more faculty.”
As you point out, reducing/eliminating waste, unevenness, and unreasonableness is the better option… An intelligent option that should appeal to all us PhDs.
Higher ed has the added problem that most faculty hate any “solution” that comes from industry and fight vigorously against the “corporatization” of higher ed. Therefore, Lean management is unattractive, even though they do not know or understand it.
Dan Markovitz via Twitter said:
See this article:
“Nurse Retention: Work Environment Issues for Nurses”
In part:
Mark,
Can you help me with best practices to accurately collect “effective hours per pt” clinically?
Thank you
AC
Hi Andy-
There are different ways to collect that data for “bedside percentage.” I think the most practical approach is direct observation and shadowing of staff. You can’t, of course, do that all day long… but you can collect data through sampling.
My recommendation is to train nurses to shadow nurses, rather than having engineers or Lean people doing it. The comfort level for the nurses will be higher and they can work together to identify process improvement opportunities as they are observing.
There are also more tech-driven approaches, such as iPhone apps that help nurses do their own time study on themselves during the day:
http://www.laubrass.com/umtplus/
Sometimes, people propose using RFID or other technologies, but I’m not sure that would really accurately measure time at the bedside(s)… possibly, but I haven’t tried that (and it might be expensive).
Mark
Thanks for feedback. Appreciate your quick response.
Mark,
Locally we are seriously considering taking % of time at bedside as a overall metric for one of our nursing services. Can you possibly provide me with a contact at Virginia Mason who could help answer some operational questions re this approach?
Much appreciated!
A couple of good tweets on this topic:
It seems, many times, that nurses just get more and more tasks added onto their workload “plate” without anything ever being removed.
Something to consider (or re-consider).
The sad reality is that ratios without the bedside nurses involved also becomes less meaningful. What we have seen without ratios, the numbers are all over the place, and the variances can be dangerous. A minimum ratio ensures we have a starting point. What we need next is a paradigm shift of not just looking at bedside RN’s as the broad-spectrum solution, but as healthcare team facilitators. What the response has been in healthcare is for ancillary positions to be pulled from the bedside. So now even with the nurses at the bedside 90% of the time, we don’t have the full extent of their licenses and education being put to the best use. We have BSN prepared RN’s doing something like blood draws and ambulating pts. which is time intensive and can be performed by someone for way less money, and education. We need to get to a place where the whole healthcare team is individualized to the needs of each patient and then add the appropriate level of staff needed. Using a systems approach will not just bring the nurse to the bedside, but give them the time to evaluate the treatment plan. We can truly see the RN become the eyes & ears of the hospital physician and alert them to emergent as well as potential issues. This will help us to deliver safer care and also help our physicians to have more time to focus on aberrancies.
Yes, proper analysis and design would make sure that nurses are doing the work that nurses should do (likewise, pharmacists are doing pharmacist work, etc.). There’s a time and a place for teamwork (not falling back on “that’s not my job”), but there’s a difference between a nurse occasionally helping with a task versus doing it all the time because there’s not enough support staff, etc.
I’m not certain that 90% bedside time is really the goal that helps optimize the entire system. What really matters is patient care. The “time at the bedside” number might have diminishing returns and, if I were managing a unit, I’d want to make sure that single number wasn’t the only goal.
Thanks for your comment!
We’ve sent people to Virginia Mason and there were some significant exclusions of time away from the bedside in their calculations. Still, they have made some remarkable changes and may be the best at that measure. We have a unit that has achieved 54% time at the bedside with still much to do.
Thanks for that reporting, BS.
Is it “apples to apples” of what they exclude from the denominator in the bedside % calculation? Did they previously exclude those same things when they had a baseline of about 30% bedside time?
My memory is failing me and I may be wrong but lunches and personal breaks were excluded. I also think that the denominator only included “time available to provide nursing care” so administrative chores, huddles(?), and other were not included. I think the national collaborative on TCAB (transforming care at the bedside) may have a more standardized definition of time at the bedside.
The broader point, that you made well, is that there is a lot of opportunity to eliminate waste and administrative overburden with all kinds of patient benefits including improved patient safety.
Thanks. It makes sense to remove planned “away time” (especially since, in an ideal environment, nurses would be able to take lunches and breaks and not have that count against some metric).
I’d personally include administrative chores, huddles, etc. in the denominator, but realizing that they should happen and it might not be realistic to get to 90% bedside time when measured that way. We should have our huddles, but if they’re going on longer than they should be or if administrative chores are taking too long (hence keeping nurses away from the patients), that’s a problem to solve (with a better countermeasure than “stop having huddles”).
See this article:
“Hospitals resolve to increase nurses’ time at the bedside” about the TCAB (Transforming Care At the Bedside) program that’s based on Lean:
Another hospital reported their results:
That’s creating far more time than hiring twice as many nurses would have. We need more of this.
Hi,
Great topic-
I am doing research on improving efficiency and eliminating waste within the Employee Health department at the hospital. i am looking at two technologies for TB testing- a simple blood test vs the traditional skin test. There is much waste of time and admin efforts to the skin test- two visits from the healthcare worker vs one visit, etc.
How do I equate the costs associated with the waste and prove one modality is more cost effective than the other. i would like to present the cost savings results back to management. Can cost analysis be transferred into a histogram to visually show management the savings?
Curious to see if anyone has experience on presenting results and in what format?
Hi-
I don’t understand how a pareto would be used here. It’s a matter of presenting tradeoffs between the two approaches. What’s the cost impact to the organization? Cost impact to the patient? Is there a revenue / reimbursement difference to consider?
There’s no magic formula, but it’s a matter of doing that research, trying to consider all factors, and then making a recommendation based on that.
Beyond financial issues, how is the quality of the two tests? Which is more patient-centered? A single visit is probably clearly better than two visits.
Mark
I am fine with less waste and a better use of nurses time. What is not factored in here is the unpredicatbility of nursing. What is assumed is all your patients will be calm, cooperative and there will be no unnessecary complications-such as needing a lift to go to the bathroom etc. Such as a code of red, blue, green or white (we have 7 but only those occur immediately at the bedside). Many studies prove more nurses do result in better patient outcomes. I agree it is better to help nurses have more time at the bedside. Parknicollet uses Kaisen. Supplies are kept in stock much better than in hospitals where it was not used. More work does need to be done in this area so everyone is safe–doctors, nurses, patients, nurses assistants, respiratory therapist etc. (the nurse usually is the coordinator of all axillary personal that have to do with the patient–including family members) reducing this job would be really helpful.
Thanks for your comment, Jean. Of course the variation of unpredictability of patient care has to be considered. That’s one reason why I usually point out that we can’t plan for everyone to be 100% busy. We have to plan for a lower average utilization to account for variation (when workloads are higher than normal or average).
See my other post on that topic:
https://www.leanblog.org/2010/08/how-to-design-poor-service-expect-100-utilization-of-people-or-resources/
Studies show that patient safety improves with more nurses. Are there similar studies that have looked at the effect of reducing waste? I’ve seen first hand how reducing waste can free up time, which reduces falls and pressure ulcers because nurses have more time for care.
More nurses is one solution. But that’s not always possible if there are nursing shortages and, arguably, reducing waste is a more financially responsible solution that can also maintain or improve quality.
[…] Why “More Nurses” Isn’t the Best Way to Solve What Ails Healthcare […]