As National Patient Safety Awareness Week continues, thanks go to Graham Foster for sending me this article from the UK: Most NHS staff deem care ‘fit for their own family'.
Well, that's a positive, happy sounding headline. “Most” think the care is good enough to recommend. But, after reading the reality expressed in the article, the headline might be construed as what that great Lean thinker Pascal Dennis calls “happy talk.”
Happy talk gets in the way of improvement when leaders are more interested in making things look good instead of actually improving the underlying system.
As a quick aside from my manufacturing days, I was told once by a Director that I reported to that his job was “my make my boss look good” (and the implication was that my job was to do the same).
As Billy Crystal used to say on SNL, it's better to look good than to feel (be) good?
OK, back to the serious work of providing health care and that article.
“Most staff deem care fit” — What does “most” mean?
Of 203,000 staff questioned for the 2013 NHS survey, 65% said care was fit for relatives, 24% were unsure, while 11% would not recommend the service.
Only 65% say the care is fit for their relatives. That means 35% are NOT willing to make that comment. Are 24% of them really unsure or just afraid to say something negative?
An alternative, but equally correct, headline could say “One third of NHS do not say care is fit for relatives.”
Let me take a time out to say that this post is NOT about knocking the NHS. These are global problems faced in healthcare – the global problems of poor quality and patient safety problems.
The problem, in England and around the world, is NOT bad people — it's bad systems.
Case in point, from the article:
And a third said they had witnessed or reported potentially harmful errors or near-misses at work in the last month.
Are things improving?
68% say in their role they are able to contribute improvements to the organisation.
That, sadly, means 32% of staff says they CANNOT contribute improvements.
At my Healthcare Kaizen co-author's has about 40% of employees who actually contribute and implement at least one small improvement each year. I'd hope if a similar survey was done, far more than 68% would they say are “able to” contribute improvements.
In general, too many patients are being put at risk (and, again, this is true in the U.S. and Canada, too). Instead of happy talk, leaders need to be willing to talk honestly about reality. Patients are being harmed. Very few healthcare leaders state this fact very directly or openly, even with their own staff. Not talking about the problem doesn't make it go away.
Back to the UK / BBC / NHS article:
Only 56% of staff said hand-washing materials – such as soap – are always available, with the figure being 59% in acute hospital trusts.
Hospitals love to put up posters that lecture the staff about washing their hands (like this, this, and this). These blaming signs imply that staff don't know about or don't care about hand hygiene. This is ridiculous.
Hospitals also sometimes make staff wear buttons that encourage patients to ask them if they've washed their hands.
But, as I've pointed out, managers are never asked to wear buttons that say “Ask me if we're out of hand gel.”
How can staff wash their hands (and protect patients) if they have empty soap containers or empty hand gel dispensers?
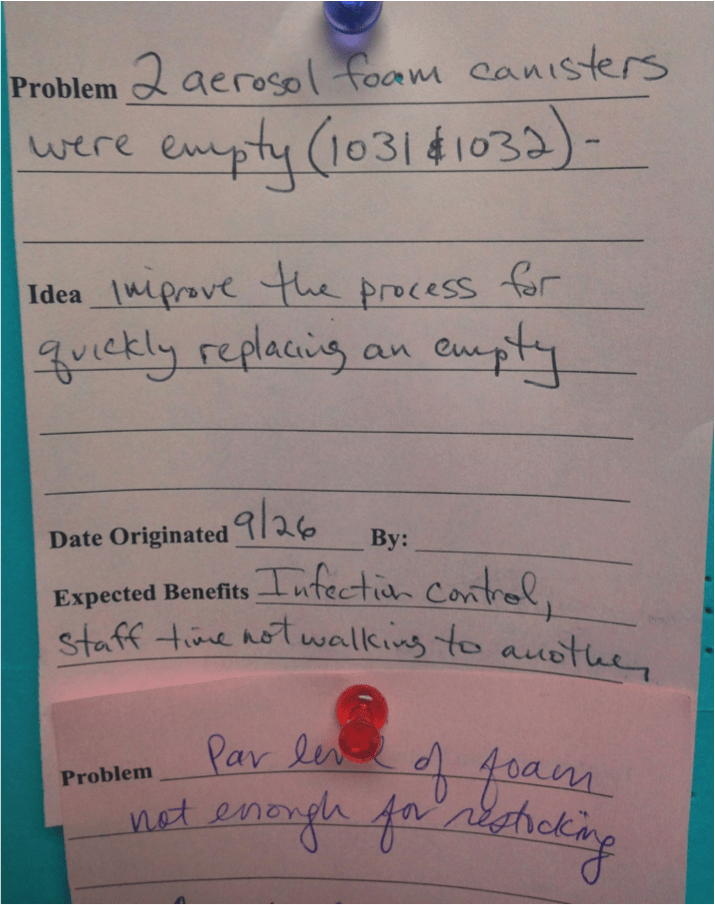
This was reported as a Kaizen problem recently at a hospital I worked with. This is a really common, widespread problem.
Whose job is it to make sure the hand gel dispensers are full? Whose job is it to make sure there's a good system and good processes that ensure these canisters always have soap or gel in them?
As Dr. Deming said, management is responsible for the system. Quality and patient safety begin in the boardroom, as he said.
We need to fix systems and processes so that staff can do the right thing for the patients 100% of the time. Hanging signs and posters doesn't fix it. Buttons and pins won't fix it. Surveys won't fix it.
Some “leaders” might lecture their staff by saying things like, “How dare you speak badly of our hospital? That's embarrassing. Don't say negative things to the media and don't make us look bad in surveys.” Do you want to sound good or be good?
If we have the right systems and processes, hospital employees might be more willing to recommend their hospitals to their family and friends.
Is the glass (and the hand sanitizer dispenser) half empty or half full?
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation:










In light of this, how prevalent in health care is reflection (hansei) ingrained in the leadership ? This seems to go to how the problem is viewed from both the leadership and the folks on the front lines.