
Since moving into healthcare in 2005, I've been surprised by a number of things in the hospital environment. The first time a skilled medical professional (a laboratory medical technologist) said, “they just want me to check my brain at the door” (true story), I was stunned. That's what GM assembly line workers said to me in 1995. It was sad then and even more heartbreaking to hear in a hospital in 2006.
Another thing that surprised me was the fairly common practice of “flexing” staff, including nurses. This typically means sending staff home early when the expected workload isn't there.
I saw a question on the online HME (Healthcare Management Engineers) group about flexing, asking in a non-judgmental way about hospitals' practices. After a few days of general silence on the rights and wrongs of the issue, I chimed in, saying (at the risk of sounding sanctimonious, I realize):
I'd argue that “flexing” should really be called something more brutally accurate like “sending staff home because we view them only as direct labor.”
There's such a lost opportunity in healthcare — nurses or other staff are sent home early… yet everyone says staff has no time for root cause problem solving or any continuous improvement efforts. There are studies that show that flexing really hurts morale because staff feel less than fully valued as professionals.
Toyota never sends hourly workers home early when there are parts shortages or other situations that mean there's no direct work to do. Supervisors engage their brains in improvement activities. Why can't we do the same with highly skilled nurses?
My source on the Toyota “never” statement comes from a discussion with John Shook. Has Toyota ever done this, sending people home early? Maybe, but my discussion with John:
Mark: “If a Toyota line were going to be down for the rest of the day, due to parts shortages or something, would Toyota send all of the production workers home?”
John: (without pause): “No.”
Toyota would train people or have them work on improvement activities. Their system supports that and people are trained how to do so.
It seems to have been taken as the new conventional wisdom in healthcare that being “efficient” means low cost, which mandates “flexing” and sending staff home early. I've tried challenging that a few times with hospital executives and I get a lot of blank stares. It's like I've grown a second head (one of which you are tempted to send home early for being unproductive… or maybe both of them!).
Now, I realize staffing to demand is a good thing. We shouldn't be always overstaffed. But we need SOME capacity and time for improvement, not just doing work.
Hospital demand and patient needs are hardly ever level loaded. It's hard to bring someone in to the laboratory for a three-hour morning shift and it might seem cruel to send a nurse home four hours early when her cost of commuting for that unexpectedly short day is just the same as a full shift.
I'm not opposed to staffing properly and I'm not opposed to cross-trained staff that can be shifted (“flexed”) to another department that needs additional staff based on patient needs. But, just sending people home early… that seems to violate the “respect for people” pillar of Toyota's management system. It also seems to violate the need to drive improvement into the workplace.
Many hospitals are trapped in this cycle (roughly, a “reinforcing loop” to the system dynamics crowd)
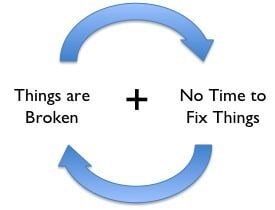
There's too much waste in the normal daily process, which interferes with proper patient care. For example, nurses can't quickly find needed equipment and supplies. But, there's no time for kaizen or continuous improvement activities. So things don't get fixed, better processes don't get put in place. Things remain broken (or get MORE broken).
When I teach hospital leaders about Lean improvement systems and employee suggestions, the first response is usually, “That sounds great, but we don't have time!!”
Maybe we would have time if we didn't rush to send nurses home the minute patient census drops. Maybe leaders are focusing too much on that sole labor productivity metric of Worked Hours Per Unit Of Service? We have labor productivity, but at what cost to quality, safety, and morale? How does length of stay suffer from this laser focus on labor cost?
Yes, I realize that labor costs are often 60 to 70% of a hospital's costs. I'm not saying to ignore labor productivity.
One follow up email on the HME discussion said this often happens:
- In the mid afternoon, patient census is low (after discharges), so RNs are sent home early (flex!)
- Then the ED has patients to admit, but there aren't enough RNs to admit them, so patients wait and care/admission is delayed
So you've saved a few hours of labor, but at what cost to the overall system? I'm sure the root of this comes down to measures and silos.
Imagine, instead, a world where RNs and Techs take time that's available when census is low to work on improvement work – little “just do its” or simple process mapping exercises. 30 minutes here, an hour there – you can actually get a lot done in small chunks of time if you do the following:
- Track improvement opportunities and staff ideas in a visual way (see my book or David Mann's
)
- Train staff and managers on Lean principles and teach them how to analyze and improve work (see the “Job Methods” program from Training Within Industry, used in healthcare circa 1945).
- Train managers on how to properly interact with staff to encourage continuous improvement (see the “Job Relations” TWI program)
- Measure results (not of each individual improvement activity) but long-term measures of the department (and broader value stream) that matter.
The alternative to “send people home” shouldn't be “let them stand around.” We need to train and motivate people (or, as Dr. Deming would say, NOT de-motivate them) and allow them to drive improvement… that's how you break that cycle and start making things better in a workplace.
Who says it can't work in healthcare? Is someone reading this willing to challenge “flexing” in their own hospital – finding the leadership required to do the training so front-line staff can start doing this?
When I worked at GM, an old UAW guy didn't want to participate in improvement efforts as he said, “I was only hired for my back and my arms.” Isn't it sad if the same is sort of true for nurses, where their brains aren't used for continuous improvement? As one person said in the discussion, “The workload is more than just direct care.”
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation:










Outstanding post, Mark! It occurs to me that the downtime could also be used for general administrative work as well, not just improvement work. Every nurse supervisor I know complains that there’s no enough time to handle all the paperwork required of her. Cross-training other nurses to absorb some of that burden means that there’s more capacity to directly deliver patient care.
BTW, the new site looks great on an iPhone!
Some quick analysis shows that at a local hospital there is about 1 hour of flex time per patient visit. At an average hourly rate of $30/hour, that is about $1 million expense for the local hospital. The center for disease control and prevention estimates 34.9 million in-patient visits or just over 1 billion dollars in additional expense to the public.
Would there be a return on investment? Maybe. Currently the leadership structure is not in place to do much with this extra staff time, nor is there a culture of continuous improvement in place in most hospitals. Flexing staff is a poor practice, but time for improvement is not the constraint.
Bean, where does that data come from?
I think the opportunity for quality improvement and cost savings are huge, it’s hard to understate how much process improvement could take place if staff were given the time, training, and leadership. Heathcare professionals are very motivated to provide the best patient care. I’ve just always been frustrated when staff are told, literally, to stop doing “that process improvement stuff” and just focus on their jobs.
Toyota always says you have two jobs:
1) Do your job
2) Improve how your job is done
Healthcare needs to focus on both of those, I’d say, not just doing your job and going home.
Bean,
As lean practitioners, we sometimes forget that “Rome wasn’t built in a day”. By this, I mean that it is our job to paint the vision for our leaders AND help show the baby steps toward that vision. I would never suggest to my hospital leadership team that we should stop flexing. You’re right in that if we don’t have capable coaches in place, this would lead to failure. However, as we develop the skills of our leaders, can’t we take baby steps toward the vision? Can’t we say “let’s stop flexing in this area over here because we have a manager who has lean thinking?” “Let’s start to learn as an organization how we might better use this time”.
Too often, as lean practitioners, we present this “pie in the sky” vision without helping our leaders to bridge that gap from where we are to “pie in the sky”. Is that their problem? Or is it ours?
Steve – you make great points. My post was admittedly a bit pie in the sky. To make my suggestion a reality certainly requires a plan and training, of staff and managers.
It’s the same thing as not just jumping into what you might call a “kaizen event” by giving people 4 days of free time without any training, direction, or context. “Report out on Friday….”, you probably wouldn’t hear much of anything reported out.
Hold on Nelly! Depending on swings in census a nurse could go months without being sent home without pay and then all of a sudden could be sent home twice in two weeks. How are you going to build “administrative work” or “continuous improvement” except at a superficial level around such real life situations.
And who says “call offs” are not in fact already built into the compensation package? I know, let’s pay 5% less and don’t send nurses home! There used to be plenty of jobs for nurses in positions that didn’t get called off (physician clinics, insurance companies, quality management, nursing homes, home health, etc) before the recent recession but many went unfilled because nurses like the glamour of hospital work, shift differentials, overtime, and yes, higher base pay too. When the economy was booming nurses were complaining about mandatory overtime and nurses could cherry pick shifts. Now when hubby or wifey lost his/her construction job and suzy/johnny nurse is now the primary bread winner of course they are going to complain.
Truth be told nurses are at least as guilty as administration in the current situatation and I might know because I am married to one and I are one.
I think two cents makes a very valid point. Before deciding to invest a whole lot of resources to train the entire nursing staff (and others) in Lean methodology and creating a bureaucratic structure to identify and track PI projects, the first step should be to see how many occurrences of sending staff home or calling them off actually does occur.
The assumption also is that being sent home early always is a negative. I can’t but imagine that there are days when some staff would welcome the opportunity to leave early to take care of things a normal work week typically doesn’t allow for.
Lastly, I would suggest using this time for nursing education programs as opposed to process improvement projects. Having to bring in addtional staff to replace staff that are taking required or competency improving training and education also comes at a cost. During a recent ICU project, the manager told me that his staff have to come in during their days off to complete these programs. I can’t imagine that that’s a booster to staff morale.
Perhaps the answer is doing a better job of baseline staffing, putting it lower so that you’re more likely to be staffing upwards instead of downwards. Of course that presumes that there is a steady availaible internal PRN pool or agency personnel to do this with, but it sure seems a far better approach than routninely staffing too high and then having to send staff home. Other options to consider should be to have “flexibility” in the application of staffing grids. There will be times when patient acuities on a give unit are such that they can allow existing staff to safely take on an extra patient or two. And, for nurse managers who routinely do not take a patient assignment, doing so on occasion is another way of being able to staff lower to help reduce the need for sending staff home.
Couple of more things. I know of one very large organization that has many union sites that don’t call off and guess what they do? They intentionally understaff and flex up with existing staff to meet increased variation in demand. Considering their base staffing levels are generally higher than industry norms this puts extreme pressure on RN to provide quality care.
Secondly, Toyota assembly plants carefully screen applicants to ensure that staff want to and are capable of contributing to quality improvement. No such screening takes place in hospitals and in fact you have a portion of your workforce that not only isn’t trained in continuous quality improvement they don’t want to!
Lastly, Philosophically and practically call offs are bad! The industry can do much better but it is a very complex issue that won’t be solved through editorilizing. Let’s identify some best practices (whoops, that would require benchmarking! Is that still a lean “no – no”?) and talk about what can be practically done in the short term to start changing the industry.
I never suggested anything bureaucratic at all. Truly daily kaizen doesn’t require a huge central infrastructure to plan week-long projects, not in the least. A lot of improvements can be handled locally and don’t take that long. Rearranging where supplies or forms are located — a lot of that can be done by a local team leader, charge nurse, and staff.
Some insightful comments made above:
1) Is flexing (sending staff home early) always received badly? Probably not 100% of the time. But from feedback I’ve gotten directly, working with nurses, it certainly seems like a net negative. Are there studies that shows it helps morale? So far, I’ve presented one study that says it hurts morale.
(link to that study)
2) Do all staff members want to participate in this? No, of course not. Do hospitals use this as a hiring criteria? Probably not, good point. Can hospitals afford to be as selective as Toyota given the nursing shortages? Probably not. Sometimes you have to be happy with technical competence, I suppose.
3) Using “free” time for nursing education seems like a great use of time, compared to sending them home. Are nurses “direct labor” or professionals? My argument is to treat them more like professionals and not like the workers who lined up in front of Ford factories looking to be hired (or not) every day in the 1930s.
4) Is editorializing going to solve it? Let’s get the NY Times and WSJ to kill their editorial pages. I’m trying to make people think and the discussion seems to indicate that’s happening.
5) There are no easy answers here.
ditto Stuart on the training and ed provided the extra person do it off the unit. At any given time during the day at least one nurse is behind on something. I don’ think it is practical to think that a nurse doing ed at the nurse’s station isn’t going to be put into patient care the first time a nurse gets behind.
I agree that FT/PT staff should not be sent home. However, I don’t think we will win the argument not to “flex” people home when volume changes. The healthcare industry is a service industry and is different than GM. In the auto industry, they adjust the workload by changing inventory levels so they can keep everyone working and changes to staffing can occur over longer periods of time. In healthcare, the volume changes (sometimes rapidly) and an healthcare organization that does not adjust will not reach its budget goals. Overstaffing would be considered a ‘waste’ under lean thinking.
But why can’t a hospital do both, flex its staff and involve them in lean / process improvement activities. The use of base (core) staff would typically consist of 80% FT/PT and 20% as supplemental. These supplemental (PRN, OT, Float, extra PT, etc) are often paid a premium for the ability of the hospital to flex them when workload is not there. Initial investiment in improvement activities (with the 80% core staff) should lead to operational savings that allow more time to improve. This would negate the need to send any core staff home (paid or unpaid).
The issues often cited as barriers is the ability to get supplemental labor. This is the area where administrative teams need to develop the necessary policies and incentives that promote the capacity for a flexible workforce.
There was an excellent presentation by Sandi Yanko at the last SHS conference with many principles in managing base and flex staffing. The article was included in the conference proceedings if you attended or know someone who did.
One challenge with always sending the flex staffing home first is that with an extended low census the flex staff find themselves with no hours and pretty quickly find a different job. Also, I am not sure I want a nurse that has been called off for a couple of months straight taking care of me or my loved one. So, even if you build in flex staffing into your model they need to be given consistent shifts even if the census drops for an extended period.
Comments on safety implications and lost revenue for hospitals that flex to extinction?
If “flexing” makes a unit understaffed or causes stress or burnout or dissatisfaction, that’s not good for patient safety or the long-term good of the hospital.
I wonder if there are formal academic studies on the connections?
[…] were using on-call shifts and sending people home early when it suited them. Hospitals call it “flexing” and I’ve been criticizing that practice on this blog since 2009 or […]
[…] The Emperor’s Sacred Cow’s New Clothes – “Flexing” Hospital Staff […]
New comment via LinkedIn after I reposted this there:
Richard Tucker: Are you seeing anything different now in 2016? I worked with one convenient care clinic that would send people home about 1pm when it slowed down, knowing that there would be an after school surge coming where they would be short staffed. We talked about keeping staff there until the taper off around 7pm. It Just did not fit their mental model. So we pulled the staff together and explained the situation. One of the nurses volunteered to leave for a couple of hours and come back because as a parent with young children it gave her an opportunity to shop without juggling the kids. Win-win for everyone.
My response:
If anything, there’s MORE pressure to send people home early. One consulting group even calls “flexing” a Lean practice. Shame on them. Toyota doesn’t send people home early. The truly Lean practice is investing in your people and your process. I bring this issue up and it shocks them because hardly anybody challenges flexing, as they think that’s the way it has to be.
[…] “The Emperor’s Sacred Cow’s New Clothes – “Flexing” Hospital Staff“ […]
[…] hospitals, here as we’re going into 2017, generate significant cost savings by sending staff home early and other traditional cost-cutting measures? Are layoffs really helping? Some CEOs have learned […]