Study: Hospital Goals Sometimes Compromise Safety
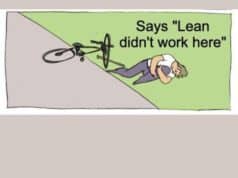
With Lean, we have realized that improving quality does not run counter to decreasing costs. They go together. Using Lean methods, improving flow, error proofing and reducing defects, leads to decreased costs in any system, be it manufacturing, healthcare, or others.
This article highlights the downside of traditional “cost cutting” in a hospital setting. Too often, traditional cost cutting means cutting heads, reducing staff, and forcing people to struggle to get by on their own accord (without improving the underlying process).
The study, published yesterday in the May issue of the journal Medical Care, found that the top hospital goals—cutting costs and improving patient safety—are “working against each other,” said senior author Dr. David Bates, chief of the Division of General Medicine and Primary Care at Brigham and Women's Hospital.
Overcrowded hospitals that are pushing too hard to streamline and cut costs are putting their patients at risk for medication errors, nerve injuries, infections and other preventable mistakes, according to a study by two Boston hospitals.
The study, published yesterday in the May issue of the journal Medical Care, found that the top hospital goals—cutting costs and improving patient safety—are “working against each other,” said senior author Dr. David Bates, chief of the Division of General Medicine and Primary Care at Brigham and Women's Hospital.
“Hospitals are clearly stressed,” he said.
A 10% increase in the patient-to-nurse ratio at one of the four hospitals studied led to a 28% increase in so-called adverse events, including infections and other injuries not caused by a patient's initial condition, Bates said.
This is sad. None of the hospitals in the study claim to have used Lean methods, I would bet that they are not. If you're not sure what changing the patient/nurse ratios means, it means cutting RN headcount. For example, instead of six patients to every RN, you now have seven patients. That means already overworked nurses are now running around more and having even less time to attend to or respond to patient needs. As it is, pre-lean RN's typically spend over 50% of their time on non-patient contact activities, much of which is pure waste or “required waste.”
Cutting staff led to quality problems. Is that surprising to anyone?
Lean is so much more effective at reducing costs. Ironically enough, with Lean, we're not focused on Cost as a PRIMARY goal. Cost is still important, but we have more constructive improvements to make other than just getting rid of people.
I don't see how increasing “adverse events” at all saves money for the hospital (and that's beyond the obvious harm and distress caused to the customer — patients and their families).
An encouraging thought:
Linda Kenney, director of Medically-Induced Trauma Support Services in Chestnut Hill, who was not involved in the study, said it highlights the fact that medical errors are a systemwide problem.
“This is not due to individuals not being caring. It's due to systems that aren't set up to do the best job possible,” she said. “When you have a nurse who has to take care of 10 patients, instead of six, things are going to be overlooked.”
Recognizing that problems are systemic needs to be a wakeup call. We can't just accept the systemic problems and say we're bound to overlook things, too bad, wish we could do better. It's imperative that we use Lean methods in healthcare to PREVENT errors from occurring. We must FIX the system rather than using the system as an excuse. It's NOT the fault of individual RN's or any individuals in the system.
What do you think? Please scroll down (or click) to post a comment. Or please share the post with your thoughts on LinkedIn – and follow me or connect with me there.
Did you like this post? Make sure you don't miss a post or podcast — Subscribe to get notified about posts via email daily or weekly.
Check out my latest book, The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation: